Introduction / Definition
Alert organisms / condition is one of a specified list of microorganisms / infections, which on identification should be referred to the IPC Lead (Infection & Prevention Committee) to:
- Investigate possible healthcare associated infection
- Address possible ongoing transmission risks by advising on control measures
- Investigate as an alert signal for a possible outbreak
Alert organism case definition must fulfill all three criteria:
- Isolation of an alert organism from anybody sites
- The patient must be admitted to the ward
- The case must be ‘Newly Identified’ ‘Newly identified’ include: Alert organism identified for the first time during current hospital admission & cases that have been identified at your site but are new case. This means that the patient was exposed and acquired another new infection.
Type Of Common Alert Organisms In Hospital
The alert organisms under surveillance are:
- MRSA (Methicillin Resistant Staphylococcu aureus)
- ESBL (Extended Spectrum Beta Lactamases)
- CRE (Carbapenem Resistant Enterobacteriaceae)
- MRO (Multidrug Resistant Organisms)
- VRE (Vancomycin Resistant Enterococci)
 |
Diverse type of alert organism |
Clinical Significance, Diagnosis and Laboratory Diagnosis
MRSA
MRSA or known as Methicillin Resistant Staphylococcus aureus is Staphylococcus aureus that tests oxacillin or cefoxitin-resistant by standard susceptibility testing methods or by a positive result for penicillin binding protein 2a (PBP2a) latex agglutination test or molecular testing for mecA gene. It may also include positive results of specimens tested by other validated polymerase chain reaction (PCR) tests for MRSA.
MRSA is especially troublesome in hospitals, prisons and nursing homes, where patients with open wounds, invasive devices and weakened immune systems are at greater risk of healthcare associated infection than the general public. MRSA began as a healthcare associated infection, but has developed limited endemic status and is now sometimes community-acquired. The terms HA-MRSA (healthcare-associated MRSA) and CA-MRSA (community-associated MRSA) reflect this distinction.
ESBL
ESBL or known as Extended Spectrum Beta Lactamase are enzymes that mediate resistance to extended-spectrum (third generation of cephalosporins e.g ceftazidime, cefotaxime and ceftriaxone) and monobactams (e.g. aztreonam). CLSI recommends confirmation of potential ESBL producing isolates of Klebsiella pneumoniae, Klebsiella oxytoca, Escherichia coli and Proteus mirabilis by performing phenotypic testing using both cefotaxime and ceftazidime, alone and in combination with clavulanic acid.
The main reservoir is the lower bowel of colonized or infected persons. Common ways of transmission is through unwashed hands. The risk factors for ESBL are extensive treatment with antibiotics, prolonged stay in a health care institution, particularly in an ICU, severity of illness (neutropaenia, organ transplant, haemodialysis or tube feeding), indwelling catheters and communal living setting. Routine screening of staffs for ESBL is not recommended. In an outbreak with ESBL producing bacteria, screening should follow a protocol to actively identify new cases.
CRE
CRE, which stands for Carbapenem Resistant Enterobacteriaceae are a family of germs that are difficult to treat because they have high levels of resistance to antibiotics. Klebsiella species and Escherichia coli are examples of Enterobacteriaceae, a normal part of the human gut bacteria that can become carbapenem-resistant. KPC (Klebsiella pneumoniae carbapenemase) and NDM (New Delhi Metallo-?-lactamase) are an example of CRE. KPC and NDM produce carbapenemase, an enzyme that break down carbapenems and many other beta lactam antibiotics, hence make them ineffective.
Healthy people usually do not get CRE infections – they usually happen to patients in hospitals, nursing homes and other healthcare settings. Patients whose care requires devices like ventilators (breathing machines), urinary (bladder) catheters or intravenous (vein) catheters, and patients who are taking long courses of certain antibiotics are most at risk for CRE infections.
Some CRE bacteria have become resistant to most available antibiotics. Infections with these germs are very difficult to treat, and can be deadly – one report cites they can contribute to death in up to 50% of patients who become infected.
Modified Hodge Test (MHT) is the screening test in detection of Carbapenemases in Enterobacteriaceae group, which using Klebsiella pneumoniae ATCC BAA-1705 (positive control) and Klebsiella pneumoniae ATCC BAA-1706 (negative control) to differentiate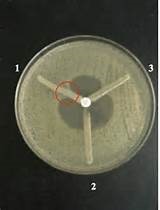 the positive and negative result for CRE.
the positive and negative result for CRE.
MHT test showing the result of CRE :
No. 1) QC positive control (Klebsiella pneumoniae ATCC BAA-1705)
No. 2) QC negative control (Klebsiella pneumoniae ATCC BAA-1706)
No. 3) Sample test (positive result)
MRO
MRO or known as Multidrug Resistant Organisms are bacteria that have become resistant to certain antibiotics, and these antibiotics can no longer be used to control or kill the bacteria.
Antibiotics are important medicines. They help fight infections that are caused by bacteria. Multidrug Resistant Organisms are found mainly in hospitals and long term care facilities. They often affect people who are older or very ill and cause bad infections. MRO develop when antibiotics are taken longer than necessary or when they are not needed. At first, only a few bacteria may survive treatment with an antibiotic. The more often the antibiotics are used, the more likely it is that resistant bacteria will develop. These MROs can go to infect peoples.
Most often, MROs spread from patient to patient on the hands of healthcare workers. They can also spread on objects such as medication cart handles, bed rails, bedside tables, IV poles and catheters. They can also spread person-to-person through direct contact (touching oozing sores, for instance). Multidrug Resistant Organisms can cause infections in almost any part of the body, including bloodstream, lungs, urinary tract, wounds and skin.
Multidrug Resistant Organism infections are hard to treat because they do not respond to many common antibiotics, even the powerful ones. But certain antibiotics can still help control MROs in most people. The doctor will try to find the type of MRO causing the illness. This can help choose the best antibiotic. Treatment with the wrong antibiotic can slow recovery and make the infection harder to cure.
VRE
Enterococci are bacteria that are normally present in the human intestines and in the female genital tract and often found in the environment. These bacteria can sometimes cause infections. Vancomycin is an antibiotic used to treat some drug resistant infections caused by enterococci. In some instances, enterococci have become resistant to this drug and thus called vancomycin-resistant enterococci (VRE). Most VRE infections occur in hospitals
People with colonized VRE (bacteria are present, but have no symptoms of an infection) do not need treatment. Most VRE infections can be treated with antibiotics other than vancomycin such as Linezolid and Tigecycline. Laboratory testing of the VRE can determine which antibiotics will work. For those people infected with VRE in their bladder and have urinary catheters, removal of the catheter when it is no longer needed can also help get rid of the infection.
Prevention & Control of Alert Organism
In general, use routine practices and contact precautions (gloves and gown) when providing direct resident care.
- Accommodation in single room with own toileting
- Good hand washing and apply My 5 moments for hand hygiene
- before touching a patient
- before clean/aseptic procedures
- after body fluid exposure/risk
- after touching a patient
- after touching with patient surroundings.
- Provide help to residents with their hand hygiene practices
- Routine environmental cleaning
- Use dedicated personal care equipment whenever possible and thoroughly clean and disinfect shared equipment
- Using Personal Protective Equipment (PPE)
- Use gloves and long sleeve gown while providing direct resident care and cleaning resident’s environment
- Routine cleaning of the environment, laundry and dishwashing
- Careful use of Antibiotics : Using antibiotics only when needed, and for the shortest time possible, helps prevent the growth or more MROs
- Monitoring: Hospitals and other healthcare facilities monitor the spread of MROs and educate caregivers on the best ways to prevent it.

Reference
- District Laboratory Practice in Tropical Countries By Monica Cheesbrough 2nd Edition (2006)
- Centers for Disease Control & Prevention (CDC) Online
- NHS – Worcestershire : Infection and Prevention Control Countywide Health Services
- Alert Organism – Scribd Online
| Last Reviewed | : | 3 March 2017 |
| Writer | : | Aliyaisma binti Ariffin |
| Translator | : | Aliyaisma binti Ariffin |
| Accreditor | : | Mohd Razali bin Hassan Sabery |