Polycystic ovary syndrome (PCOS) is a condition that may affect a women’s menstrual cycle, fertility and in some cases physical appearance. The commonest complaint among women with PCOS is menstrual disorder or irregularity, and this is largely due to hormonal imbalance and anovulation. The failure to ovulate regularly leads to problems with fertility or difficulty in getting pregnant. PCOS is also associated with higher circulating levels of male hormones or androgens in the body and this may lead to hirsuitsm or excessive facial hair growth, acne, and/or male-pattern hair thinning. However, it should be noted that excessive facial or body hair can also be genetic as seen in some races.
PCOS is a relatively common disorder affecting about 5 to 10 % of women in the reproductive age group.
A large majority of women with PCOS are overweight or obese and there is a higher risk of developing diabetes, obstructive sleep apnea and other long term health risks (see complications below). Women with PCOS should be screened for diabetes.
PCOS is one of the commonest cause of infertility or difficulty in getting pregnant. However, there are available medications that could induce regular ovulation and help them to conceive.
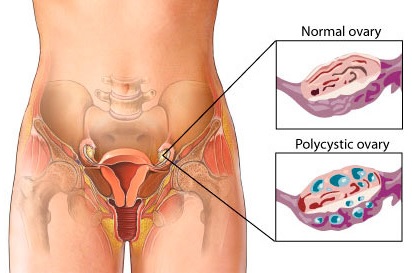
What are polycystic ovaries?
Polycystic ovaries are usually slightly larger than normal in size and ultrasound imaging will show multiple small cysts within the ovary. Polycystic ovaries are quite common and may be evident in up to 20% of women. However, having polycystic ovaries does not necessarily mean you have polycystic ovary syndrome. Several other clinical features as described in this article should be present. Approximately, only 6 to 7% of women with polycystic ovaries have PCOS.
Cause
The cause of PCOS is still unknown. However, it may run in families. Women with PCOS has abnormal levels of the pituitary hormone luteinizing hormone (LH) and high levels of male hormones (androgens) which interfere with normal function of the ovaries.
In women with PCOS, multiple small cysts (4-9 mm in diameter) develop in the ovary. None of these small follicles are capable of growing to a size that would trigger ovulation. As a result, the levels of estrogen, progesterone, LH, and follicular stimulating hormone (FSH) become imbalanced.
Insulin is a hormone which regulates the level of glucose (a type of sugar) in the blood. Women with PCOS may not respond to insulin (known as insulin resistance) and this may result in higher levels of glucose. In response to this, the body produces more insulin. High levels of insulin may lead to weight gain.
Symptoms of PCOS
The symptoms may vary in terms of severity. Some may only have mild symptoms, while others are more severely affected
The symptoms of PCOS may include:
- irregular periods or no periods at all,
- difficulty becoming pregnant (reduced fertility),
- having more facial or body hair than usual (hirsutism),
- loss of hair on the head,
- overweight or obesity,
- oily skin and acne,
- depression and mood swings.
Women afflicted with PCOS may have present with different signs and symptoms at different times. Some of the signs and symptoms are quite common among the general population, making it relatively difficult to diagnose. A diagnosis of PCOS is usually made when the women have any two of the following:
- irregular, infrequent or no periods,
- more facial or body hair than is usual and/or blood tests show higher testosterone levels than normal,
- ultrasound scan which shows polycystic ovaries.

Ultrasound image showing a polycystic ovary
Treatment
The management of women with PCOS need to be tailored according to the presenting signs and symptoms. Does she want to conceive? Is hirsuitsm a problem? Does she require treatment to prevent endometrial hyperplasia (abnormal thickening of the inner lining of the womb) or possible cancer of the womb?
Oral contraceptives – (OCs; with combined estrogen and progestin) are the most commonly used treatment for regulating menstrual periods. OCs protect the woman from endometrial hyperplasia and cancer of the womb (endometrial cancer). Certain OCs that contains anti-androgens (e.g. cyproterone acetate) may also effective in preventing hirsutism and acne.
Progestin – a hormone called progestin (e.g., Provera) for 21 days every one to three months. This will induce a period in almost all women with PCOS, but it does not help with the hirsutism and acne neither prevent pregnancy. It does reduce the risk of cancer of the womb and endometrial hyperplasia.
Hirsuitism – Excess hair growth on the face and/or other parts of the body can be removed by shaving or use of depilatories, electrolysis, or laser therapy. Many women worry that these treatments cause hair to grow faster, although this is not true (See Hirsutism). There are medications available to reverse or treat hirsuitism. This medication have anti-androgens effect (e.g. cyproterone acetate or alderone) but it has to be taken at least a 4 to 6 months and the woman must be on an effective family planning method, as pregnancy is contraindicated during the treatment.
Weight loss – Weight loss is one of the most effective approaches for managing insulin abnormalities, irregular menstrual periods, and other symptoms of PCOS. By losing 5 to 10% of body weight, periods may become more regular. Weight loss can often be achieved by program diet and exercise. Referring the patient to a dietician would be useful.
Metformin – Metformin (Glucophage) is medication that improves the effectiveness of insulin produced by the body. It may benefit in selected cases of PCOS who has anovulation. Women with PCOS, diagnosed to be diabetic should be managed accordingly.
Infertility – management options are available in women who do not ovulate regularly;
- Weight loss – 5-10% of weight loss may allow the woman to begin ovulating normally.
- Clomiphene (anti-estrogen) – an oral medication used to stimulate follicular development and ovulation
- FSH injections – given if a woman does not ovulate with clomiphene or fail to conceive
Complications
PCOS can give greater risk of developing long-term health problems which include:
- Insulin resistance and diabetes: 10–20% women with PCOS go on to develop diabetes in the future. Risk of developing diabetes is increased further if the woman is over 40 years of age, have relatives with diabetes, developed diabetes during a pregnancy or obese (body mass index or BMI over 30).
- High blood pressure: Hypertension is likely to be related to insulin resistance and being overweight, rather than the PCOS itself. Hypertension can lead to cardiovascular disease and should be managed appropriately.
- Heart disease in later life: it is linked to health conditions such as diabetes, high blood pressure and high cholesterol level.
- Cancer: With short periods (less than three a year), the endometrium (lining of the womb) can become abnormally thick and this may lead to endometrial cancer in a minority of women. Women in the reproductive age group with no periods or infrequent periods should seek medical attention. PCOS does not increase a women’s chance to getf breast, cervical or ovarian cancer.
- Depression and mood swings: It can lower self-esteem.
- Snoring and daytime drowsiness: PCOS can lead to fatigue or sleepiness during the day. It is also associated with snoring.
How to reduce these complications?
The main ways to reduce the overall risk of long-term health problems are to have a healthy lifestyle:
- healthy balanced diet. Take more fruits, vegetables and whole-meal foods (such as whole meal bread, whole grain cereals, brown rice, and whole-wheat pasta), lean meat, fish and chicken. Decrease sugar, salt, caffeine and alcohol.
- eat meals regularly including breakfast
- take exercise regularly (45 minutes at least three times a week).
- aim to keep weight to a normal level (a BMI between 19 and 25).
- By losing weight, the women will have a lower risk of developing diabetes and cardiovascular disease (heart problems). They may also regain regular periods which will reduce the risk of endometrial cancer and improve her chances of getting pregnant.
- Have regular health checks: to check for any early signs of health problems. Women with PCOS above 40 years old, a blood sugar test once a year should be offered to detect development of diabetes. However, if she is obese (BMI over 30) or have a family history of diabetes, then testing for diabetes should be done earlier than the age 40 is recommended.
Conclusion
PCOS is a common problem affecting young women. It is a difficult problem to treat, but attaining normal weight and living a healthy lifestyle is an effective way of controlling the condition. The medical management of PCOS should be tailored based on the presenting complaint and medical issues.
References
- Legro RS et al. Clomiphene, metformin, or both for infertility in the polycystic ovary syndrome. N Engl J Med 2007; 356:551.
- Huber-Buchholz MM et al. Restoration of reproductive potential by lifestyle modification in obese polycystic ovary syndrome: role of insulin sensitivity and luteinizing hormone. J Clin Endocrinol Metab 1999; 84:1470.
- PCOS, what it means for your long-term health. The Royal College of Obstetricians and Gynaecologist, UK 2009.
| Last Reviewed | : | 23 August 2019 |
| Writer | : | Dr. Hj. Mohamed Hatta b. Mohamed Tarmizi |
| Accreditor | : | Dr. Haris Njoo Suharjono |
| Reviewer | : | Dr. Rafaie bin Amin |







