What is vitiligo?
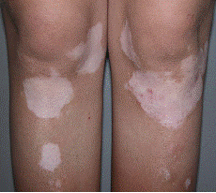
Vitiligo is a common skin disease affecting 0.5-2% of the population. It is characterized by well circumscribed, depigmented (white) spots on the skin and is usually symmetrically distributed (Figure 1). Approximately half of the patients acquire the disease before the age of 20 years and about 1/3 have a positive family history. It can also be associated with other autoimmune diseases such as diabetes mellitus, thyroid disease, pernicious anaemia and Addison’s disease. Vitiligo can be classified into 5 types-generalized, focal, segmental,acrofacial and universal. Generalized vitiligo or vitiligo vulgaris is the commonest type.Diagnosis is usually made clinically, although a skin biopsy may be helpful in some cases.
|
|
|
|
Figure 1 |
|
-
Vitiligo affecting both legs, symmetrically distributed
-
Vitiligo affecting the right arm
Treatment of vitiligo
There is no definitive cure available and the aim of the treatment is to achieve repigmentation of the lesions and stabilize depigmenting process.
Treatment can be divided into:
- General treatment
- Topical treatment
- Phototherapy
- Surgical treatment
In general, topical treatment is suitable in patients with localized vitiligo, phototherapy in patients with generalized involvement and surgical treatment in patients with segmental vitiligo.
General treatment
- Photoprotection – A sunscreen is recommended to protect the vitiligo skin from sunburn and koebnerisation (where vitiligo lesions developed on the site of trauma/sunburn).
- Avoidance of trauma – This minimizes koebnerisation.
- Camouflage – Cosmetics and skin dyes can be used to mask the lesions, especially if they are extensive and causing psychological distress.
Topical treatment
- Topical corticosteroid.
It is most useful for localized vitiligo of recent onset. It is the first line therapy for children and face lesion has the best response. Potent topical corticosteroid has the highest success rate. If no response is seen after 3 months, alternative therapy should be sought. - Topical tacrolimus.
This may be indicated in younger patients and for sensitive areas of the skin such as eyelids, as it does not produce atrophy and other adverse effects associated with topical steroid. - Depigmentation.
This involves irreversible bleaching of normal skin. It is only considered in patients with extensive vitiligo who have failed all other forms of treatment. 20% monobenzylether of hydroquinone is applied to the skin until the skin is bleached.
Phototherapy
- NBUVB (Narrow band UVB).
Studies have shown that NBUVB is more effective than oral or topical PUVA in achieving repigmentation and has fewer side effects. Treatment is given 2-3 times a week. It is safe in pregnant women and children. - Topical PUVA (Psoralen +UVA).
0.1% 8-methoxypsoralen (MOP) is applied to the vitiligo skin and exposed to UVA after 30 minutes. Treatment is given 2-3 times a week. Adverse reactions that require temporary discontinuation of therapy include excessive redness, blistering, oedema and intense pruritus. Topical 8-MOP and sunlight exposure can be given to patients who have difficulties in accessing UVA phototherapy. - Oral PUVA (Psoralen + UVA).
It is indicated in more extensive involvement or in patients who do not respond to topical PUVA. It is contraindicated in pregnant and breastfeeding women, children < 12 yrs old, photosensitivity disorder, history of skin cancer or cataract. Oral 8-MOP is given 2 hours before exposure to UVA. Treatment is given 2-3 times a week. Side effects include nausea, vomiting and phototoxic reactions. - Excimer laser.
This has been reported to achieve clinical improvement and can selectively treat vitiligo patch, sparing the non-affected areas.
| Last Reviewed | : | 23 August 2019 |
| Writer | : | Dr. Azura Mohd Affandi |
| Accreditor | : | Datuk Dr. Roshidah Baba |
| Reviewer | : | Dr. Nazatul Shima bt. Abd Rahim |