Encephalitis is defined by the presence of an inflammatory process of the brain tissue in association with clinical evidence of neurologic dysfunction.1 Meningoencephalitis is an inflammatory process involving both the brain tissue and meninges2 (Figure 1)
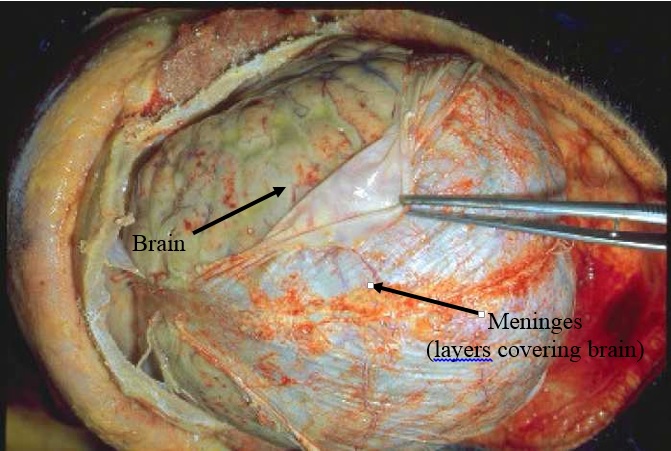
Figure 1
The estimated annual incidence of encephalitis in the UK is 4/100,000. Infection in adults can also be very severe2. Of the pathogens reported to cause encephalitis, the majority are viruses.1
Aetiology
Herpes simplex virus is a severe direct viral infection of the brain with a serious sequalae. Other viruses that may act the same way are herpes zoster, EBV, CMV, enteroviruses, adenoviruses, rabies, and Japanese B encephalitis.
Indirect infection of the brain as a result of an autoimmune reaction after patient infected with certain viruses may occur;Influenza, measles, rubella, varicella, and HIV.
Secondary or primary infection with other organisms may occur with tuberculosis, mycoplasma, listeria, Lyme disease, cat scratch fever, leptospira, brucella, legionella, neurosyphilis, and all causes of bacterial meningitis.
Others:
- Rickettsial: Rocky Mountain spotted fever, endemic typhus, epidemic typhus, Q fever.
- Fungal: cryptococcosis, coccidiomycosis, histoplasmosis, candidiasis.
- Parasitic: trypanosomiasis, toxoplasmosis, echinococcus, schistosomiasis, amoebiasis.
However, despite extensive testing, the aetiology of encephalitis remains unknown in most patients1.Another major challenge for patients with encephalitis is to determine the relevance of an infectious agent identified outside of the CNS; these agents may play a role in the neurologic manifestations of illness but not necessarily by directly invading the CNS.1
Signs and symptoms
Acute rapid progression of meningoencephalitis may begin with a simple flu-like illness or with a headache, followed by rapid development of altered consciousness, with confusion, drowsiness, seizures and coma.
Subacute presentation were related to symptoms of increased intracranial pressure such as severe headache , vertigo, nausea , episodes of convulsions and clouding of mentation.
Other significant symptoms were photophobia, sensory changes and neck stiffness.
Clinically, there will be evidence of clinical seizures, focal neurological signs and cognitive impairment.2
Complications
Acute2
- Cardiac and respiratory arrest.
- Metabolic derangement.
- Intractable seizures
- Secondary bacterial infection in blood and lungs.
- Disseminated intravascular coagulopathy (DIVC).
Long term2
- Emotional and psychological disturbance
- Impaired memory
- Physical problems include mild imbalance, co-ordination and dexterity problems or major neurological problems with speech and swallowing problems and total dependency.
Treatment
Empirical therapy
Although a wide range of viruses have been reported to cause encephalitis, specific antiviral therapy for viral encephalitis is generally limited to disease caused by the herpesviruses, especially herpes simplex virus. Because the earlier treatment is started for herpes simplex encephalitis, the less likely that death or serious sequelae will result. Acyclovir (10 mg/kg intravenously every 8 h in children and adults with normal renal function) should be initiated in all patients with suspected encephalitis as soon as possible, pending results of diagnostic studies.
Other empirical antimicrobial agents should be initiated on the basis of specific epidemiologic or clinical factors, including appropriate therapy for presumed bacterial meningitis if clinically indicated.1
Specific therapy
Following the identification of a particular microorganism (by antibody studies, molecular methods, or culture) in a patient with encephalitis, appropriate antimicrobial therapy or management should be initiated.1
Prevention
- Vaccination for Japanese encephalitis and rabies.2
- Vector control for Arbovirus.2
References
- Alan et al, The Management of Encephalitis: Clinical Practice Guidelines by the Infectious Diseases Society of America,Clinical Infectious Diseases 2008;47:303–27
- www.patient.co.uk/encephalitisandmeningoencephalitis/2012
| Last reviewed | : | 28 August 2020 |
| Writer | : | Dr. Mohd Sufian b. Adenan |
| Accreditor | : | Dato’ Dr. Hj. Md Hanip b. Rafia |
| Reviewer | : | Dr. Nor Faizah bt. Ghazali |







