Definition
Neonatal jaundice (also called icterus) is a condition characterized by the yellow discoloration of the skin and sclera (whites of the eyes) of newborn infants. Neonatal jaundice is the most common reason for readmission to hospital in the first week of life. It occurs in nearly 70% of full term babies. Premature babies have much higher incidence of neonatal jaundice. Neonatal jaundice is a result of the deposition of bilirubin, secondary to increased bilirubin levels in the blood, a condition known as hyperbilirubinemia.
Bilirubin results from the breakdown of hemoglobin in the red blood cells. It exists in unconjugated form which is insoluble in water and is transported to liver by plasma albumin. In liver, it is then converted to conjugated bilirubin which is much more soluble in water. The conjugated bilirubin is then excreted into the bile.
Neonatal hyperbilirubinemia may result from various conditions, some of which are transient such as neonatal physiological jaundice of the newborn while some are more serious conditions that cause sustained hyperbilirubinemia in the newborn. Neonatal physiological jaundice results from increased RBC breakdown and immature neonatal liver. It is not harmful, often appears in 2 to 4 days old baby and disappears by 1 to 2 weeks of age. Prolonged jaundice often indicates a serious condition in neonate, such as hemolytic disease of newborn, biliary atresia or in rare situations, idiopathic neonatal hepatitis.
Laboratory Investigation
Management of jaundiced neonates often requires only observation and serial blood tests for Total Bilirubin. For further investigation in certain cases, the testing for bilirubin fractions is required. The blood Bilirubin is usually measured as both Total Bilirubin (TBil) and Direct Bilirubin (DBil). Total Bilirubin is the sum of the direct and indirect forms. The indirect fraction is obtained by subtracting the DBil from TBil. Direct bilirubin correlates with conjugated bilirubin whereas indirect bilirubin correlates with unconjugated bilirubin.
Sample collection and handling
Blood can be obtained from neonates’ veins or heel. A repeat sample may be requested due to insufficient volume, contamination or other factors. The above techniques require drawing of blood causing pain and trauma to the neonate and therefore in some healthcare facilities, non?invasive transcutaneous photometric measurement at point of care using a dedicated instrument ‘bilirubinometer’ is used in infants in lieu of blood drawing.
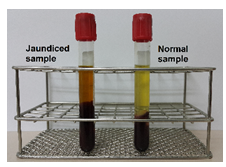
Bilirubin is photosensitive, and the blood samples should be protected from light for accuracy. Exposure of samples to light or heat may cause degradation of bilirubin and reduce its concentration. The blood sample should be sent immediately to laboratory for testing as delays in transportation of blood samples can also influence the bilirubin test results. The serum/plasma of jaundiced sample appears darker (brownish), as shown in the diagram.
Determination of Bilirubin level helps the physician to ascertain the underlying mechanism for the hyperbilirubinaemia. Hence accurate and unbiased measurement of Bilirubin becomes mandatory. Listed below are few analytical methods which are used in laboratory for determination of Bilirubin level :
- Direct spectrophotometric method
Absorbance is measured with a dual-wavelength narrow bandpass spectrophotometer. Neonatal Total Bilirubin can be determined from the difference in absorbance at these two wavelengths.
- Diazo methods
Bilirubin is most commonly measured based on the principle of Diazo reaction method reported by Hijmans van den Bergh, in which diazotized sulfanilic acid (Ehrlich’s diazo reagent) reacts with bilirubin to produce pink to reddish-purple coloured azodipyrroles that can be measured calorimetrically. In aqueous solution, the water soluble, conjugated bilirubin reacts rapidly with the reagent and is said to be “direct-reacting”. However, when methanol is added, both conjugated and unconjugated bilirubin are soluble and react with the reagent, providing the total bilirubin value. The unconjugated bilirubin, which is much less soluble in aqueous solution and can be measured only after the addition of methanol, the term “indirect-reacting” is applied.
- High performance liquid chromatography (HPLC)
HPLC methods allow for relatively rapid separation and quantification of the bilirubin fractions. A newer highly accurate method of estimation involves alkaline methanolysis of bilirubin followed by chloroform extraction of bilirubin methyl esters and later separation of these esters by chromatography and spectrophotometric determination.
However, for diagnostic purposes, the use of direct and indirect diazo techniques provides sufficient clinical information.
Limitation of test / Interference factor
Dietary pigments such as carotene will falsely elevate Bilirubin level measured by direct spectrophotometric method. However, dietary pigments generally not present in neonates due to their limited diet. The diazo method of Bilirubin estimation is inaccurate in detecting low levels of Bilirubin. In particular, direct measurements over estimate Conjugated Bilirubin at low concentrations and underestimate it at higher concentrations. Thus in some cases, slight elevation of Unconjugated Bilirubin failed to be identified, which is of value in detecting conditions like Gilbert syndrome.
Reference Range:
| Age | Total Bilirubin Level | |||
| Full Term | Premature | |||
| mg/dL | mmol/L (SI unit) | mg/dL | mmol/L (SI unit) | |
| 0 -1 day | <5.0 | <86 | <4.0 |
<68
|
| >1 day | <8.0 | <137 | <6.0 |
<103
|
In general, the normal reference range of Total Bilirubin, Conjugated Bilirubin and Unconjugated Bilirubin for newborn from 0 to 7 days are listed below:
Total Bilirubin : 1.0-10.0 mg/dL or 17-170 mmol/L
Conjugated (Direct Bilirubin): <0.8 mg/dL or <13.6 mmol/L
Unconjugated (Indirect Bilirubin): < 10.0 mg/dL or < 170 mmol/L
Importance of laboratory test
Elevated Bilirubin level in neonates can diffuse into basal ganglia and cause toxic encephalopathy (kernicterus) due to their immature blood-brain barrier. Kernicterus is characterized by the yellow staining of the lipid-rich meninges of the brain and spinal cord. It typically occurs at Bilirubin levels greater than 20 mg/dL( 342 mmol/L) in infants and may result in death, cerebral palsy, deafness or mental retardation. Hence infants who develop jaundice need close monitoring and severe neonatal jaundice requires immediate medical attention.
References
- Arneson, W.L., &Brickell, J.M. (2007). Clinical Chemistry: A Laboratory Perspective. Philadelphia: F.A. Davis Company.
- Champe, P.C., Harvey, R.A., & Ferrier, D.R. (2005). Lippincott’s Illustrated Reviews: Biochemistry (3rded.). Baltimore: Lippincott Williams & Wilkins.
- Puppalwar, P.V., DrKalyanGoswami, &Dr. ArchanaDhok. (2012,Sep-Oct).Review on “Evolution of Methods of Bilirubin Estimation”.IOSR Journal of Dental and Medical Sciences (IOSRJDMS), 1(3), 17-28
- Fischbach, F.T., & Dunning III, M.B. (2009). A Manual of Laboratory and Diagnostic Tests (8thed.). Philadelphia: Wolters Kluwer Health|Lippincott Williams & Wilkins.
- Murray, R.K., Granner, D.K., Rodwell, V.W., Bender D.A., Mayes, P.A., Botham, K.M., et al. (2006). Harper’s Illustrated Biochemistry (27thed.). New York: The McGraw-Hill Companies, Inc.
- SaththaSivam, P., Voralu, K., NoraidaRamli, Mohd Rafi Mustapha, Julia Omar, & Van Rostenberghe, H. (2010, Jul-Sep). The effect of delayed transportation of blood samples on serum bilirubin values in neonates. Malaysian Journal of Medical Sciences, 17(3), 27-31.
| Last Reviewed | : | 31 January 2016 |
| Writer | : | Lee Kie Hie |
| Accreditor | : | Lau Kim Bee |