Introduction
Ionizing radiation is widely used in medicine, industry, agriculture and research. It provides invaluable benefits. However, radiation sources can be lost, stolen, or otherwise not under proper control, and this can lead to injuries to people who come into contact with them.
The usage of radiation for medical purpose is based on the principle that it produces sufficient benefit to offset any possible the radiation detriment to the irradiated person. The main aim is to make sure that the magnitude of individual doses, the number of people exposed to radiation and the likelihood that possibly exposures will actually occur should all be kept As Low as Reasonably Achievable (ALARA), economic and social factors being taken into account. The use of IR for medical purpose is well regulated by the existing Atomic Energy Licensing Act 1984 (Act 304), subsidiary regulations, standards and guidance documents.
An emergency is a sudden and unexpected occurrence that may have an adverse effect not only on the organization, but also to the surrounding community. An emergency often occurs when organizations are not fully prepared to deal with it immediately and this makes things worse.
A radiation emergency is a critical situation in which there is, or is perceived to be, a hazard from unwarranted exposure to ionizing radiation. Medical radiation emergencies include incidents involving sealed and unsealed radioactive sources, and radiation generators. Radiation accidents may cause health effects if the radiation dose is above the threshold deterministic effect. This may cause injuries and eventual death. There is also a risk of stochastic effects from radiation exposure which may cause cancer and severe hereditary effects. In any emergency immediate steps must be taken to minimize the radiological risk to the patient, worker and public.
Why Radiation Emergency Response Plans should be established?
Any emergency requires immediate reaction as in the time of emergency; a small incident can turn into a crisis, if proper action is not been taken to control it. In other words, emergency response management process involves the initial preparation to face any eventuality, reduce or limit the impact, respond to the circumstances or events that may occur, and recovery after an emergency incident.
The medical response team must be prepared and trained to adequately treat injuries caused and complicated by ionizing radiation exposure and radioactive contamination. There should be established and designated hospitals that have medical professionals who have been trained and are experienced in dealing with radiation injuries. Efficient and fast medical response is necessary in any medical radiation emergency. Nuclear detonation and other high-dose radiation situations are the most critical (but less likely) events as they result in acute high-dose radiation.

Figure 1: Radiation burn on both hands (taken on February 23, 2000), Samut Prakan (Thailand)
Medical Response Plan
In any event of a radiation emergency, the medical response will depend on whether there has been exposure to external sources of radiation or contamination with radioactive material; the number of victims and the severity of the injuries. The usual principles of medical care apply at the scene of the emergency as at a hospital, but the details and type of radiation emergencies may differ.
In a medical radiation incident, both workers and members of the public may be exposed to ionising radiation from:
- Unshielded or shielded source(s);
- Radioactive sources (e.g.radionuclides) deposited on the ground or other surfaces;
- Radioactive sources (e.g.radionuclides) contaminating the body, clothing or possessions, and
- Inhalation or ingestion of radioactive substances as a result of direct atmospheric or environmental contamination or, subsequently, by radioactive material in water or food.
Medical managing of an emergency situation is generally divided into medical care on-site (more often for workers) and medical care off-site (for workers and for affected population).
The basic principles of the medical handling of exposed persons are based, to a large extent, on the techniques used for handling other types of accidents, taking into account the possible effects of radiation and contamination to health. Exposed persons with high levels of external dose will be unusual and more often than not will be among the employees or other professionals. In the case of a lost or stolen source, restricted groups of the general public may get doses that can lead to deterministic health effects. Such a situation needs specialised medical care for the early effects of acute radiation and palliative treatment where necessary.
In the planning stage of the medical response plan the following lists should be prepared:
- List of medical facilities at the local, regional, and national levels;
- List of specialized medical facilities in other nearby countries;
- List of medical and support staff with telephone numbers and addresses in each respective location;
- List of specialised medical centres for treating patients with radiation induced skin lesions or immunosuppression;
- List of supplies and articles needed for emergency response, and agreements with ambulance transport services where necessary;
- List of radiation monitoring and medical physics related equipment
Medical Response Organization in the Event of a Radiation Emergency
According to the Prime Minister’s Directive 20 of the National Security Council, the leading technical agency for any radiation emergency will be the Atomic Energy Licensing Board (AELB). The MOH will be responsible for providing medical care to the victims while the control of environmental spread of radioactive substances, assessment of its impact on the environment, food and water supplies, properties and the initiation of protective measures for these items will be the responsibility of the AELB.
Medical preparedness must begin with awareness of where and what type of ionising radiation and radioactive materials are used in the country. This information database should include at least:
- Locations where radiation or radioactive materials are used;
- Categories and activities of radioactive sources;
- Types of radiation generating devices;
- Information regarding the transportation of radioactive materials through any respective area;
- Spectrum of possible accidents, and
- Estimation of the number of persons potentially affected in a severe radiological accident.
All this information is necessary for adequate planning of medical capabilities. General and specialised medical centres may also be needed, depending on the degree and nature of radiation induced injuries. Specialised advice may not be routinely available at the scene of the accident, except at medical facilities, such as medical irradiation therapy hospitals, where there are medical professionals who are experienced in dealing with radiation injuries or who have some knowledge in this respect. The Ministry of Health Malaysia (MOH) has to ensure that plans exist to provide treatment; monitoring and health advice to the public and to persons who may have, or fear they may have been contaminated or exposed to radiation (Fig 3).
The state Health Department would act initiate emergency response in the event, and will co-manage the team in providing assistance to the authorities, the information will be notified to the hospital for so on. They also provide information to the public regarding safety measures (Fig 2)
The MOH is responsible for providing advice to other Ministries and Government departments on the health implications of any exposure to radiation and is also responsible for ensuring that plans exist to provide treatment, monitoring and health advice to the public. There are three levels of response, according to the degree of complexity, with respect to the necessary resources for assistance and the severity of consequences:
|
Table1. Radiological Response Organization
|
|
|---|---|
|
Personnel Role
|
Function
|
| Medical Response Initiator | Responsible for obtaining basic information characterizing the emergency and notifying the appropriate level of response. |
| First Responder | First person or team to arrive at the scene of an accident with an official role to play in the accident response. |
| Emergency Response Team | The ERT is the specialized medical team responsible for providing first aid to casualties |
| Public Health Division | Responsibility of the Public Health Division in a radiation emergency is to advise the public about possible threats and initiate the response public communication |
| Emergency Medical Manager | Is responsible for managing the actions of the Hospital Emergency Department Response Team, the Medical Specialist of the appropriate service, the Medical Physicist, and the Radiation Protection Team. |
| State Health Physicist | Responsible for assisting the Public Health Division to initiate Radiological Emergency Response at the state level. Providing Technical Support for hospital MP during a radiological emergency |
| Hospital Emergency Response Team | A group of specialists and trained support staff from the hospital who will be notified to initiate the necessary action on the casualties arriving at the hospital. |
| Other teams | Including Bioassay, Radiopathology, Bio dosimetry, Dosimetry Teams and Medical Physics team collaboration in order to providing support during radiological emergency |
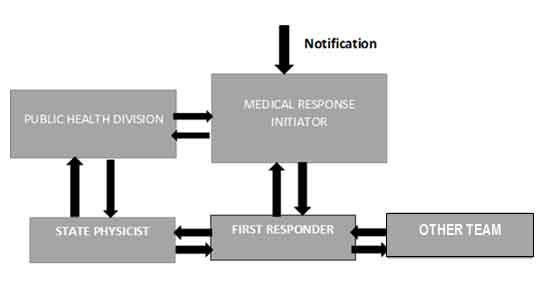
Figure 2: Medical response organization for State Health Department
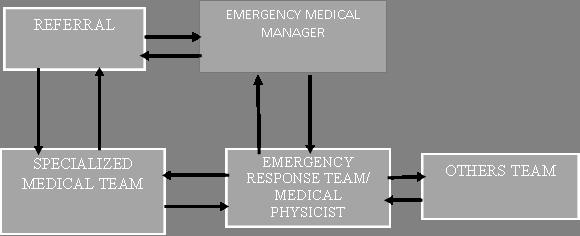
Figure 3: Medical response organization for hospital level
Medical handling in an emergency situation is normally divided into medical care onsite (more often for workers) and medical care off-site (for workers and for affected population). To organise the medical response it is recommended that the system for Medical Assistance for Radiation Emergencies be under the supervision of the Ministry of Health. The general structure of the system is shown in Fig (4)
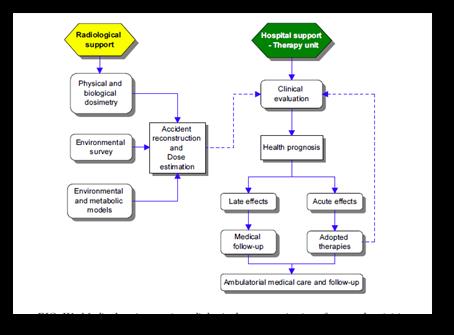
Figure 4: Medical Assistance in Radiological Emergencies: Interface and Activities
The Ministry of Health is responsible for providing advice to other Government departments on the health implications of any exposure to radiation. It is also responsible for ensuring that plans exist to provide treatment, monitoring and health advice to the public and to persons who may have, or fear they may have been contaminated or exposed to radiation.

Figure 5: Checking radiation sources – exercise
The important issue in an emergency is to address the protection of the staff members and first responders. Workers should be monitored for radiation exposure and the risk of health effects must be kept in perspective to allow for optimal evaluation and care of victims. Healthcare workers should adhere to appropriate guidelines and standard precautions to avoid radiation injuries from handling contaminated patients.
Properly functioning radiation monitoring equipment must be immediately available in the emergency department and the staff should be sufficiently trained to perform basic radiation surveys. Basic radiation observation should focus on identifying the presence of radiation, protecting staff and patients, and controlling the spread of contamination.
All staff should adhere to the general radiation protection principles:
- Time – Minimize time spent near radioactive source
- Distance – Maximize distance from source
- Shielding – Place physical shields around source
Additionally, during an uncontrolled situation, providers should observe universal precautions, including splash and water protection. Furthermore, staff actively attending contaminated patients should wear personal monitors, such as real-time dosimeters and/or film badges, unless the level of exposure is known to be negligible.
Medical staff dealing with contaminated persons should use protective clothing (overalls, masks, plastic gloves, overshoes as required), personal dosimeters and should be monitored for possible contamination. Contaminated clothing should be carefully removed and discarded in well-marked plastic bags. Dry decontamination using a towel may be a practical way to decontaminate a person if access to showers is not possible. Otherwise, contaminated individuals should shower, using mild soap as required washing off the contamination. If the hair is heavily contaminated, cutting it off may be the simplest and most effective solution. Decontamination should be generally repeated until measurements indicate background levels.
At the national level it is necessary to provide specialised assistance to victims with acute radiation syndrome or serious radiological injuries of the skin. For this purpose it is necessary to indicate beforehand highly specialised hospitals with various departments (Haematology, Haemotherapy, Intensive Care, and Plastic Surgery) and develop agreements to treat highly exposed persons at such hospitals.
Medical staff and support personnel should be trained on the principles of radiation protection, health consequences of the exposure and methods for dealing with exposed and/or contaminated persons. The training should include drills and exercises in medical response and in performing contamination monitoring, decontamination, interviews, etc.
The management at every designated medical facility is responsible for the following aspects:
- Designation and, if necessary, additional training of appropriate staff;
- Development of detailed emergency plans and procedures;
- Indication of space where reception and treatment can take place, and
- Provision and proper maintenance of special equipment and all necessary items
References
- The following scenarios are adapted from medical management of radiological casualties handbook (jarrett, 1999)
- Generic procedures for medical response during a nuclear or
Radiological emergency iaea, vienna, 2005 - Arrangements for preparedness for a nuclear or radiological emergency iaea, 2007
- Method for developing arrangements for response to a nuclear or radiological emergency, epr-method, iaea, vienna (2003).
- Guidance document on radiological emergency preparedness for medical physicists, ministry of health malaysia, 08.10.2015.
- National security council directive no. 20, policy and mechanism of national disaster management and relief
http://www.adrc.asia/management/mys/directives_national_security _council.html
| Last Reviewed | : | 06 May 2016 |
| Writer | : | Hendra Pawitra Sudarjajat |
| Accreditor | : | DR. Pirunthavany a/p Muthuvelu |







