Introduction
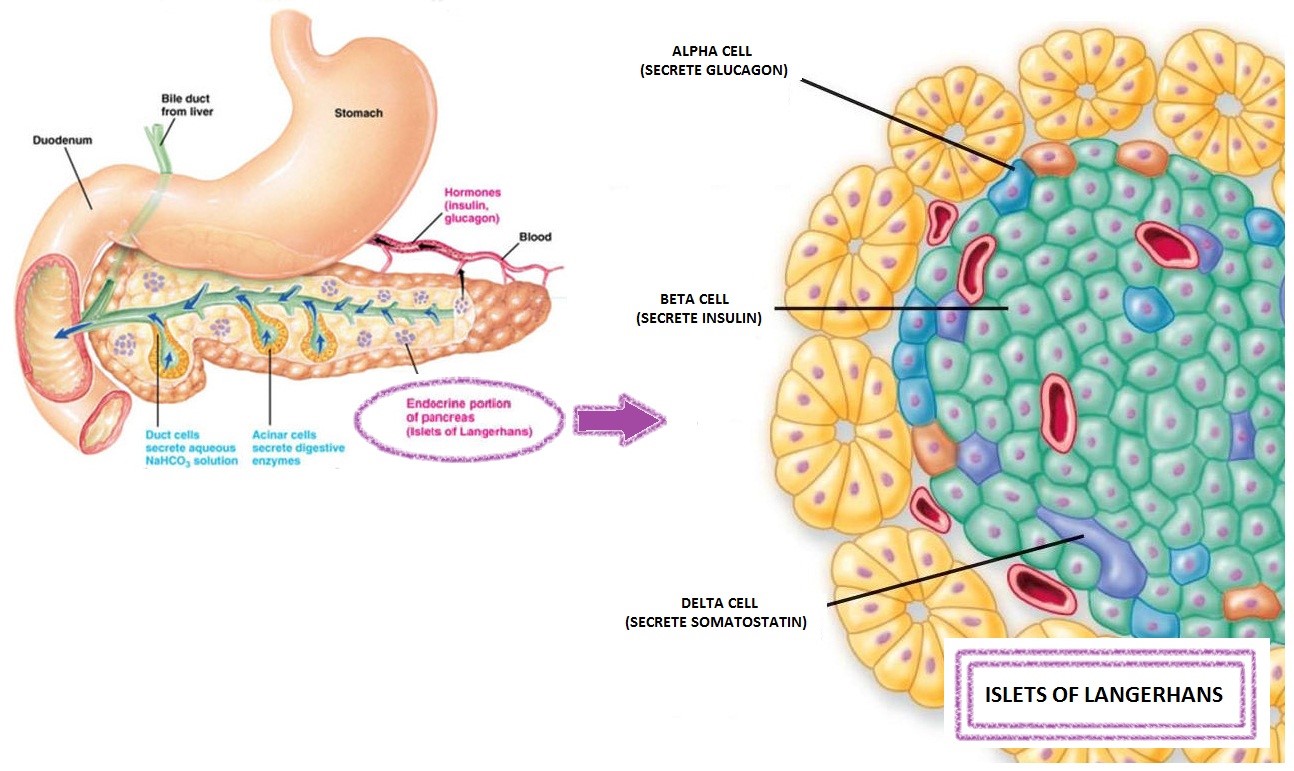
Insulin is a hormone secreted by the beta cells of the pancreas. Insulin is stored inside the beta cells of the pancreas which known as Islet of Langerhans. In our body, function of insulin are;
- Regulation the uptake and utilization of glucose
- Regulation protein synthesis and triglycerides storage
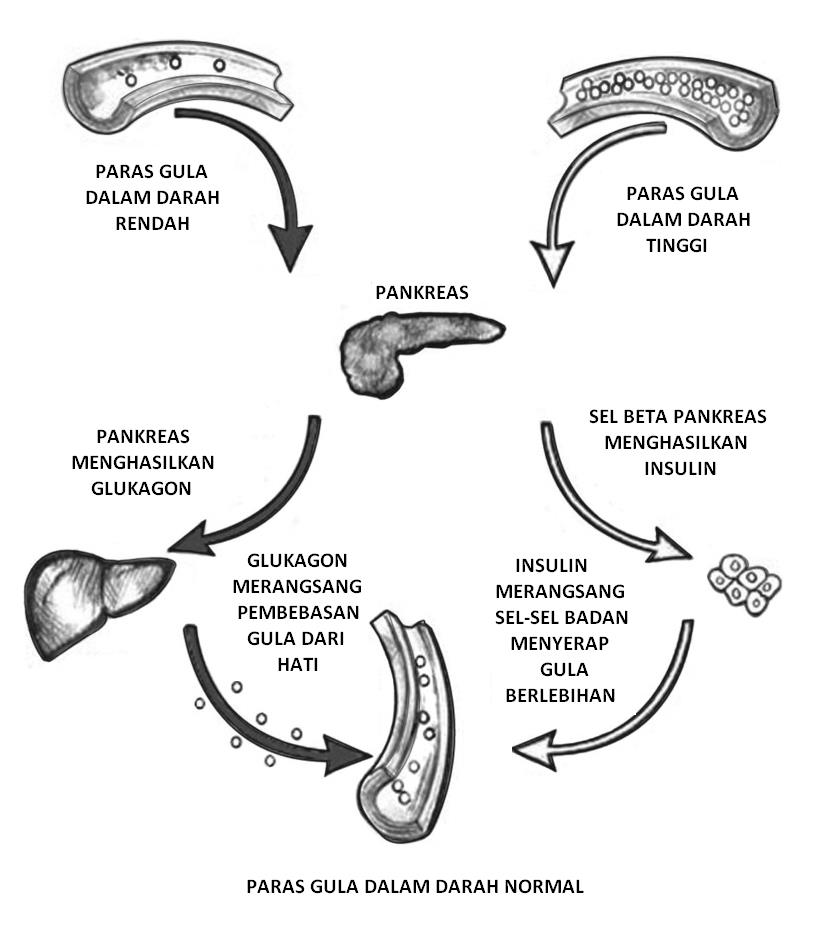
Main role of insulin is to regulate glucose level in the blood from persistently rising (hyperglycemia) or persistently low (hypoglycemia). Insulin level and glucose level must be balance in our body.
After a meal, carbohydrates usually are broken down into glucose and other simple sugars. This causes the blood glucose level to rise and thus stimulates the pancreas to release insulin into the blood. Insulin acts to stimulate the body’s cells (muscle and fat cells) to absorb sugar found in the blood for energy or be stored as glycogen and insulin will act to inhibit the breakdown of glycogen to glucose in the liver into the blood until blood sugar levels in the blood back to normal.
When blood sugar levels dropped, insulin stimulates the pancreas to secrete the glucagon. Glucagon acts to convert complex sugars stored as glycogen in the liver and muscle tissues, into simple sugars so that the level of sugar in the blood return to normal.
Insulin levels affect the production and storage of carbohydrates, fats and proteins in the body. Insulin is involved in the absorption of these nutrients by the cells of the body and used for a variety of uses such as supply of energy to the muscles of the body, repairing the muscle tissues that have been damaged, and supplying cell membrane with essential fatty acids.
Uses of Insulin Measurement
- To help evaluate insulin production by the beta cells in the pancreas
- To help diagnose the presence of an insulin-producing tumor in the islet cells of the pancreas (insulinoma)
- To diagnose insulinoma, to confirm the successful removal of the tumor and / or monitor if there is still a tumor in the pancreatic beta cells
- To help determine the cause of low blood glucose (hypoglycemia) which usually occurs in infants and children and also occurs among adults
- To help identify insulin resistance
- To help determine when a type 2 diabetic might need to start taking insulin to supplement oral medications
Patient preparation
Depending on patient diagnosis, and this will be informed by the clinician before procedure; its either;
- Patient shall fast for eight hours
- Patient do not need to fast
- Patient shall fast more than eight hours
Specimen collection, handling and storage
- The blood specimen should be collected in EDTA tube (purple cap) or either SST II tube (yellow cap) by using routine precaution for venipuncture.
- Within two hours after centrifugation, tranfer at least 500 uL of a cell-free sample to a storage tube. Tightly stopper the tube immediately.
- If the specimen is not processed immediately after centrifugation, the specimen should be stored as following;
- Store sample tightly stoppered at room temperature (15 – 30?C) for no longer than eight hours
- If the assay will not be completed within eight hours, refrigerate the sample at 2 – 8?C
- If the assay will not be completed within 24 hours, or for shipment of samples, freeze at – 20?C or colder. Thaw sample only once.
Method for insulin measurement
Method:
Method used to measure insulin level in the blood is immunoassay method. An immunoassay is a biochemical test that measures the presence or concentration of a macromolecule in a solution through the use of an antibody or immunoglobulin. The macromolecule detected by the immunoassay is often referred to as an analyte.
Factors that could affect the test results are insulin which is either through injection or is taking orally. Therefore, this information should be communicated to the medical officer in charge in order to avoid errors in diagnosis.
There are numbers of immunoassay method to measure insulin level in the blood.
- ELISA (Enzyme-linked immunisorbent assay) – is a test that uses antibodies and color change to identify a substance. This antibody is linked to an enzyme, a substance containing the enzyme’s substrate is added to detect color changes in the substrate.
- Radioimmunoassay (RIA) – RIA technique is an extremely sensitive and specific requiring specialized equipment. It used to measure concentration of antigens by use of antibodies. However, the test is expensive and require special precautions and licensing, since radioactive substance are used.
Alternative method:
For someone who has obesity or polycystic ovarian syndrome (PCOS), insulin tolerance test test (ITT) is the best method to measure insulin levels in the blood. The test involves an IV-infusion, with subsequent measurement of glucose and insulin level. This tests is one method for determining insulin sensitivity (or resistant).
If someone has developed antibodies against insulin, especially as a result of taking non-human (animal or synthetic), these can interfere with insulin testing. In this case, a C peptide may be performed as an alternative way to evaluate insulin production. This test also suitable for those with low blood glucose level (hypoglycemia) or for people with diabetes type 1.
Interference and limitation
- Hemolysis specimen containing enzyme-degrading insulin production which may causing falsely low result.
- Patient with obesity or overweight with diabetes are usually resistance to insulin. Therefore, measurement of insulin may be falsely high due to resistancy of body cells to against insulin.
- Insulin intake or insulin theraphy through injection may causing falsely high result. This is due to formation of anti-insulin antibody.
Expected result
13.0 – 161 pmol/L
Interpretation of result
|
INSULIN LEVEL
|
INTERPRETATION
|
|---|---|
| High (Hyperinsulinemia) |
|
| Low |
|
References
- American Association for Clinical Chemistry 2001-2015
- Association for Clinical Biochemistry 2012
- Beckman Coulter; Access Immunoassay System – Ultrasensitive Insulin
- Endocrinology Fifth Edition; Mac E. Hadley
- http://www.nlm.nih.gov/medlineplus/diabetestype2.html
- https://labtestsonline.org/
- Myrene et al (2010). Insulin Assay Standardisation. Diabetes Care. 2010 Jan; 33(1): 205–206.
- Remy Sapin (2007). Insulin Immunoassays: Fast Approaching 50 Years of Existence and Still Calling for Standardization. Clinical Chemistry May 2007 vol. 53 no. 5 810-812
| Last Reviewed | : | 22 May 2016 |
| Writer | : | Nurul Ain bt. Mohd Ishak |
| Accreditor | : | Nur Afiah bt. Abd Rahim |







