What is the cause of absent vaginal opening in a girl?
Imperforate hymen
- In female infants, there is normally a thin membrane (hymen) that surrounds the vaginal opening.
- In rare conditions, a congenital vaginal blockage occurs due to an imperforate hymen. Therefore the vaginal opening remains covered.
Labial adhesions
- Fusion of labial skin extending from the posterior fourchette towards the urethral opening. A thin membrane can be seen in the midline.
- Occurs in 3% of the pre-pubertal girls with peak incidence in the first year of life.
- The aetiology is unknown but lack of oestrogen may probably contribute to its occurrence.
Anomalies of the vagina
The vagina is a muscular canal connecting the cervix of the uterus to the vulva.
- Vaginal agenesis
- Absence of the vagina (vaginal agenesis) occurs when the vaginal plate fails to form vagina during intrauterine life.
- It is also known as mullerian aplasia or Mayer-Rokitansky-Kuster-Hauser syndrome (congenital absence of the vagina with variable uterine development)
- It affects approximately 1 in every 5,000 female infants
- It usually occurs with absence of uterus/cervix but presence of normal ovaries. The patient without uterus will not menstruate and cannot become pregnant. With the presence of normal ovaries, patient can have normal breast and pubic hair development.
- It may be associated with other malformations, such as:
- Kidney abnormalities in 25-50% of patients (absence of one kidney or the dislocation of one or both kidneys, fusion of two kidneys forming a horseshoe-like shape)
- Skeletal abnormalities in 10-15% of patientsaffecting the spine, ribs or limbs
- Urinary tract abnormalities. The urethra can open into the vaginal wall or the vagina can open into a persistent urogenital sinus
- Rectal abnormalities (vaginorectal fistula, vulvovaginal anus, rectosigmoidal fistula)
- Other less common anomalies include congenital heart lesions, abnormalities of the hand, deafness, cleft palate, inguinal or femoral hernias.
- Vaginal atresia or absence of the lower vagina
- The lower portion of the vagina is replaced by fibrous tissue
- Usually associated with normal development of the ovaries, uterus, cervix and upper vagina
- Surgical reconstruction is the treatment
- High transverse vaginal septum
- Occurs due to incomplete canalization of the vagina during development
How does a patient with vaginal abnormality present?
Though absence of vaginal opening may be detected early during neonatal period, it can also go unnoticed until pubertal years.
Imperforate hymen
- In affected infants, they may have bulging introitus mucocolpus (due to accumulation of vaginal secretions in response to maternal oestradiol). If the diagnosis is not made, the mucus gets reabsorbed and the child remains asymptomatic until menarche. The girl may present during adolescence with cyclical abdominal pain or pelvic pain due to haematocolpus(accumulation of menstrual blood in the vagina).
Labial adhesions
- Most infants are asymptomatic.
- Some may have urine pool behind the vaginal adhesions and cause post-micturition dribble, soreness and vulval irritation.
Vaginal agenesis
- Vaginal agenesis is typically not diagnosed until puberty (around age 15) because the external genitalia appear normal from birth
- Usually the young girl notices that she has not had her menstrual period and seeks medical attention
- A subgroup of patients may be diagnosed during infancy during which the abnormality detected during an examination or test for other unrelated problems
Importance of accurate diagnosis:
- Vaginal agenesis can potentially be misdiagnosed as an imperforate hymen, and attempts at hymenotomy may result in secondary scar formation. This can lead to treatment difficulties in the future.
- Labial adhesions must be differentiated from other paediatric vaginal disorders to avoid unnecessary intervention causing anxiety to a child and her
How to diagnose this condition?
Physical examination
- Patients with imperforate hymen may be diagnosed during neonatal period. An abdominal swelling (vagina filled by secretions from the cervical glands in response to the mother’s hormones) may be felt during physical examination.
- The diagnosis of labial adhesion can be made on examination alone and usually no investigations are indicated.
- Patient with vaginal agenesis generally have normal appearance of the external genitalia. In place of the vagina, there can be a small pouch or dimple that is I – 4 cm in depth.
Investigation
- Ultrasound may be done to check if the uterus and ovaries are both present. Ultrasound can confirm mucocolpus/hydrocolpos (abnormal swelling of the vagina) or hydrometrocolpos (abnormal swelling of both the vagina and uterus).
- In patients with vaginal agenesis, intravenous pyelography may detect congenital urinary tract abnormality and radiography may be needed if skeletal abnormalities are suspected.
How to treat?
Treatment depends on the cause of the vaginal blockage.
Labial adhesions
Spontaneous resolution is common. Treatment is usually not necessary in the absence of symptoms.
Oestrogen cream can be used topically at the midline of the fusion for a short duration of not more than 6 weeks. It will cause the membrane to separate but recurrence after discontinuing treatment is common. Prolong use is not allowed as oestrogen can cause breast swelling and tenderness. Surgical separation is rarely needed unless urinary symptoms are persistent and oestrogen therapy has failed. Recurrence is common even after surgery.
Imperforate hymen
The urologist will make a simple incision that does not require anaesthesia. Once drainage occurs, the anatomy should be examined for other abnormalities.
Vagina with high transverse septum
Surgical correction depends on its thickness and location.
Vaginal agenesis
Generally the treatment for this condition includes psychosocial support and medical/surgical correction of the anatomic abnormality. Strong support and counseling and psychological preparation before treatment is very important to ensure satisfactory outcome. A normal sex life is possible. Since the condition is usually associated with absence of uterus, the patient will be unable to carry a pregnancy.
Support and counseling for a child with vaginal agenesis:
Professional counseling of the patient and her parents should be provided timely after the condition is diagnosed. This will help them to cope with issues of gender/sexual identity and uncertainty.
The patient should be informed that she was born with a vagina that did not develop completely and not “born without a vagina”.
Emphasis should be placed on the female features and functions that the child has and not on the abnormality. The child and her parents should be reassured that the health care team can help them achieve a good outcome.
Patient should be reassured that a “more functional” vagina can be developed with the help of the health care team. Avoid using the term “artificial vagina” in the communication.
When vaginal agenesis is diagnosed during adolescence, the girl may react with shock and inability to accept the condition. She may fear rejection. The patient and her parents should be reassured that she can achieve normal development of breasts, pubic hair, vulva and clitoris. The patient should be reassured that a normal sex life is possible.
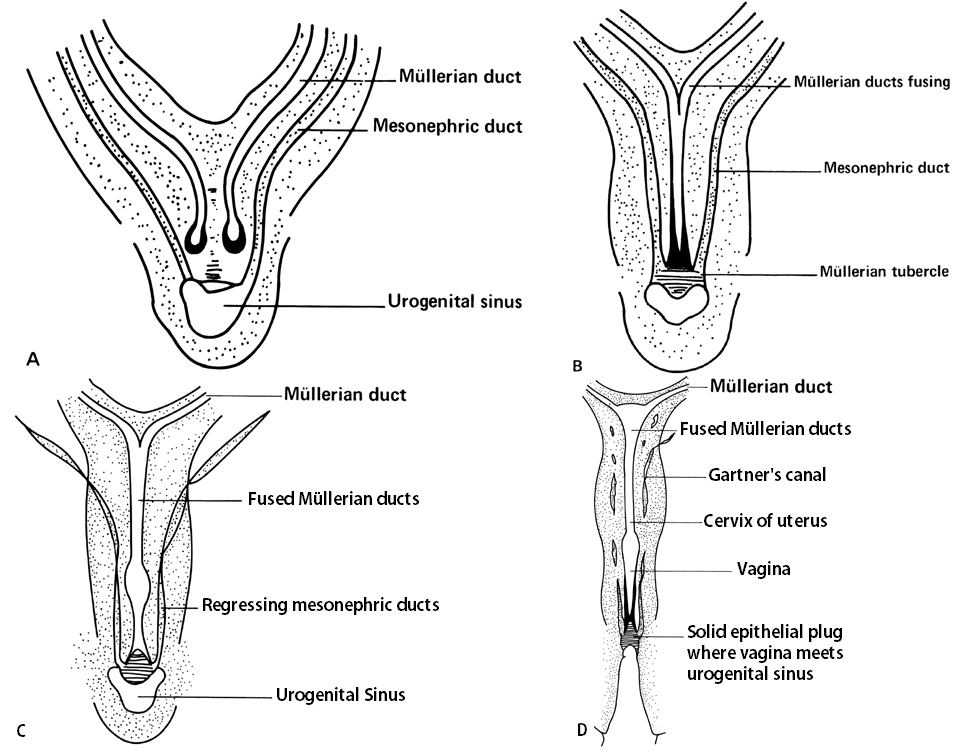
Figure1: A. Müllerian and wolffian ducts. B. Fusion of müllerian ducts. C. Regression of mesonephric ducts. D. Uterus, cervix, and vagina.
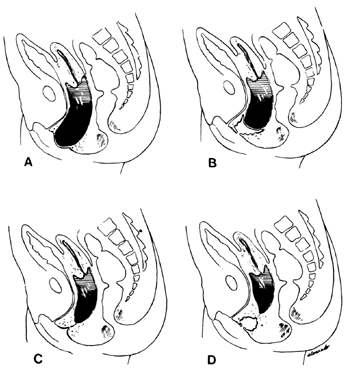
Figure 2: Diagram of various lesions causing hydrometrocolpos. A. Imperforate hymen. B. Transverse septum. C and D. Low and high atresia of vagina.
Reference:
- Handbook of clinical pediatric endocrinology. Charles G.D.Brook and Rosalind Brown. First Edition 2008. Blackwell Publishing. ISBN-978-1-4051-6109-1
- Paediatric Endocrinology, the requisites in Pediatrics. Thomas Moshang, First Edition 2005. Jr. Elsevier Mosby. ISBN 0-323-01825-4
- Urology Care Foundation. The official foundation of the American Urological Association. urologyhealth.org Muckle, C, Feinberg, E, Glob. libr. women’s med., (ISSN: 1756-2228) 2008; DOI 10.3843/GLOWM.10002
- Spencer R, Levy DM: Hydrometrocolpos: Report of three cases and review of the literature. Ann Surg 155: 558, 1962.)
- Labial adhesions. Kenneth G Nepple et al. Medscape. emedicine.medcape.com
| Last Reviewed | : | 28 August 2020 |
| Writer | : | Dr. Janet Hong |
| Accreditor | : | Dr. Fuziah bt. Md. Zain |
| Reviewer | : | Dr. Zainab bt. Kusiar |







