Introduction
Assisted Reproductive Technology (ART) basically means a procedure done to assist couples to conceive whereby the fertilization happens in vitro or outside the human body and later the embryo is transferred back into the womb. This is usually performed for couples having subfertility as a result of significant female pelvic disease such as severe endometriosis, tubal disease or severe male factor or as a result of failed fertility treatment such as intrauterine insemination.
History
This procedure was initiated nearly 50 years ago but the first successful IVF baby was only born in 1978. Subsequent to that there has been substantial advancement.
Procedure
Currently there are two common procedures being done that is in-vitro fertilization (IVF) and intra-cytoplasmic sperm injection (ICSI). In both situations the lady undergoes ovarian stimulation to form many ovarian follicles. This is mainly done using injections and the follicular growth is monitored via transvaginal ultrasound examination. The injections are usually given under the skin and occasional blood tests are done to monitor the hormonal levels. Following the follicular growth a minor surgery is done whereby the follicles are aspirated using an ultrasound guided needle which goes through the vagina into the ovary.
This procedure is usually done in an operation theatre which has an ART laboratory nearby or next to it. The presence of oocytes(eggs) are identified in the follicular fluid and are kept in the incubator. The husband’s semen is processed and the healthy sperms are collected. In IVF each egg is incubated together with a proportion of sperms, making natural selection still possible. Whereas in ICSI the egg is cleaned and directly injected with a normal looking viable sperm. ICSI requires more sophisticated equipment and expertise. It is essential in severe male factor where only a few sperms are obtained. The fertilization rate is usually better with ICSI but the drawback is there is no natural selection.
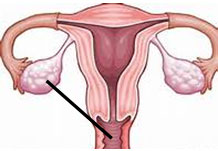
The embryos are assessed daily to ensure the level of growth and are graded by appearance. Generally one to three embryos are transferred two to three days later. The transfer procedure is similar to an IUI procedure whereby the embryos are placed in a fine catheter and this is inserted into the womb usually under ultrasound guidance. The remaining embryos are frozen for future use. The lady is usually given medication to support the pregnancy and confirmation of pregnancy is done two weeks later.
 |
 |
|
| Figure 1: Egg collection | Figure 2: Embryo transfer |
Technology advancement
There have been further developments mainly in the aspect of freezing the embryos, supporting the embryos to an advanced stage (day 5 embryo – blastocyst) and genetic testing.
Success rate
The overall success rate varies depending mainly on maternal age and other contributing factors. Generally one third to half will conceive. The rates drop with increment in the maternal age and in most centers it is not offered after the maternal age of 42. The other factors include severe male factor where there could be genetic abnormality in the male partner or in the sperm. Obesity has a detrimental effect on the final outcome.
Risks
There are risks involved, mainly ovarian hyperstimulation syndrome, multiple pregnancy associated risks and other pregnancy related issues. In ovarian hyperstimulation syndrome there is formation of multiple ovarian follicles resulting in enlarged ovaries with collection of fluid in the peritoneal cavity. If severe the fluid can extend into the lung space resulting in difficulty in breathing requiring ventilator support. As the fluid drains out of the blood circulation into these cavities there is an increased risk of blood clot formation. Therefore ART involves extensive counselling, detailed assessment and monitoring.
| Last Reviewed | : | 20 January 2014 |
| Writer | : | Dr. Kannappan a/l Palaniappan |







