Why is oral health important for people with autism?
Autism spectrum disorder is a developmental condition that affects the ability of an individual to communicate and interact with others and how they adapt to their surroundings. People with autism also have restricted, repetitive patterns of behaviour or interest. They usually like to follow a fixed routine and any disruption to this routine often results in disruptive behaviours.
Due to their uniqueness, people with autism require special approach for oral health care. Prevention of dental disease is of utmost importance for them due to a number of reasons.
Firstly, good oral health – a clean mouth, free of cavities and gum disease, promotes general wellbeing. The person is able to smile and people around them will also have no qualm in showing their affection towards them. Poor oral hygiene can lead to bad breath and pain or discomfort due to cavities or gum disease. People with autism may not be able to express their discomfort and leads to delayed diagnosis and treatment. >> Non-verbal signs of toothache
Having good teeth is also important for everyday activities such as chewing, swallowing and talking. The food that we eat needs to be properly chewed in order to assist digestion, absorption of nutrients and prevention of constipation. Certain sounds that we make require the presence of teeth, such as ‘C’, ‘S’ and ‘F’. Good dentition may help in speech development for people with autism.
Furthermore, good oral health prevents the need for dental treatment which can be very challenging for people with autism. Due to their special characteristics, people with autism may find it extremely difficult to cope with a dental visit let alone sitting in the dental chair for treatment.
Challenges for oral care:
Home oral care is the foundation to good oral health. However, many parents or carer find it difficult to perform oral hygiene care for people with autism due to behavioural issues such as refusing to open mouth, biting on toothbrush, turning the head away and aggression. They may find it difficult to cope with such ‘intrusion’ into their mouth or changes to their routine, hence all the unwanted disruptive behaviours. As a result, oral care becomes a burden to both parties.
Apart from that, some people with autism may be taking certain medications to control their mood or for other medical conditions such as seizures and gastric reflux. These medications may cause side effects related to oral health such as dry mouth, risk of tooth decay, tooth wear and gum enlargement.

Picture showing a generalized gum enlargement due to poor oral hygiene and medication intake.
Tips for parents or carer:
- Be creative
If the development of motor skills is adequate, persons with autism may brush their teeth on their own. In order to assist them, pictures containing a step-by-step brushing technique may be placed in the bathroom. >> Toothbrushing

Source: http://www.mayer-johnson.com/autism-article3
An example of visual schedule to guide a person to tooth brushing.However, some people with autism require hands-on assistance from their parents or carer. If the child is not familiar or has always been resistive to a toothbrush, try to introduce the toothbrush again in a different way. The use of pictures or videos is particularly useful. Slow but repeated exposure to the oral care aids such as toothbrush and toothpaste will help the person accept oral care more readily.
Some people on the autism spectrum have sensory sensitivities which is highly variable. For example, some people are sensitive to touch, taste and/or texture. They may dislike the feeling of toothbrush in their mouth. Some may dislike the mint flavour or the jelly-like texture of a certain type of toothpaste. Strategies that can be used include starting oral care with oral massage, followed by cleaning with a wet cloth (clean) before using a toothbrush. Other ways include using a soft bristle toothbrush or allow the child to brush his/her lips prior to entering the mouth. Try to look for the best aids that suit the individual needs of the person.
- Tell-Show-Do technique
First, tell the child that you are going to brush his/her teeth. Then show them how your will be doing it, either by demonstrating to them, or by showing a picture or video. Then perform oral care on them slowly and gently. >> Intellectual Disabilities and Oral Care
- Set a routine
As people with autism like a fixed daily routine and dislike changes, it is helpful to allocate a specific time for oral care. It is advisable to brush teeth at least twice a day- morning after breakfast and night before bed. It is also a good practice to clean the mouth after taking medications. A picture timetable is useful to help them comply with the new routine.
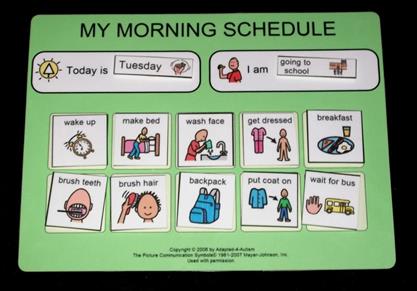
Source: http://thr7.com/daily-schedule-template-for-kids-with-autism.html
Example of picture timetable.
- Contact the nearest dentist who is trained to treat people with autism
Regular check-up at the dentist is important to ensure everything is in good condition and no dental disease has gone unnoticed. It is advisable to look for a dentist who is trained in this area and who shows interests in treating people with autism. Most dentists are trained during their undergraduate program to see patients with special needs, but the degree of exposure differs. Discuss with the dentist about the needs of the person with autism. Agree on strategies that will make the first dental visit a pleasant one.
- Preparation prior to the first dental visit
Parents and carer are encouraged to prepare the person from home a few days prior to the dental visit. Strategies include telling story about a dental visit, showing a picture story book, telling them procedures that will be undertaken, instruments that will used and smells to expect.
Discuss with the dentist, a kit containing the pictures of the dentist, dental staff and dental office and some dental items such as gloves and mouth mirror may be available for them to familiarize prior to the dental visit.
Picture of the dentist and dental team
Example of diagrams to prepare a person with autism for the first dental visit. Readers are welcomed to print this table for own use. Discuss with the dentist, photographs may be taken of the dentist and dental team to be included in this table.
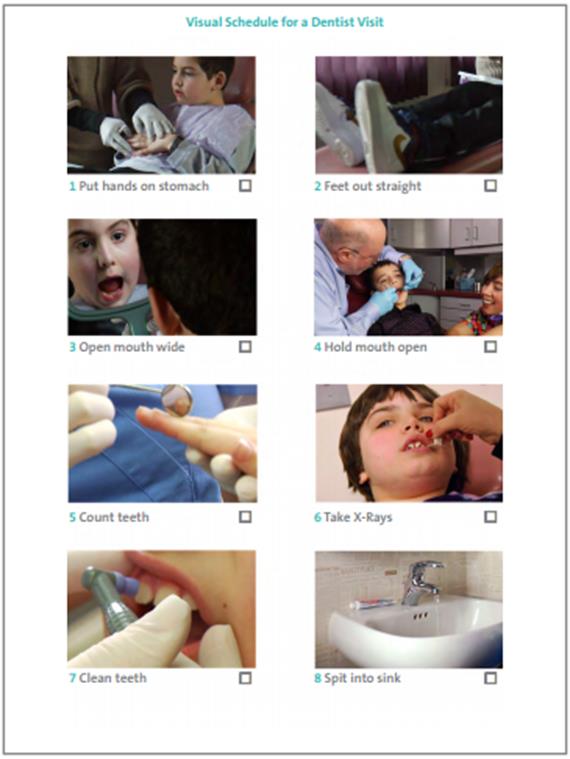
Example of picture guide to prepare a child prior to a dental visit.
(Source: https://www.autismspeaks.org/sites/default/files/documents/dentalguide.pdf)It is advisable to make the appointment early in the morning so that the child is feeling fresh and the dentist is not in a rush.
Parents or carer should be calm as well, since their own behaviour has an impact on the child’s behaviour.
- The first dental visit
Do not place too much expectation during the first dental visit. The aim of this visit is for the child to get familiarized with the people in the clinic and its surroundings. It is also the time for the dental team to know the child. Inform the dentist about the likes and dislikes of the child. A brief oral examination may be achieved but do not be discouraged if this is not the case. The child simply needs more time.
- Subsequent visits
People with autism dislike unpredictability and deal with it poorly. In order to assist them, the dentist will usually introduce a step at a time, starting with a simple procedure and slowly moving on to more complex ones. For example, the dentist may just start with tooth brushing and topical fluoride application. This if followed by introducing hand instruments before starting on machine operated instruments as the child gets more comfortable. This process may take a long time and may need several dental visits. It also requires patience and cooperation from both parties.
Sometimes, is it impossible to achieve satisfactory cooperation from the child despite all efforts by the dentist and parents/carer. In this case, the dentist may suggest dental treatment under general anaesthesia, especially if the child comes with active dental disease in the mouth. Dental treatment under general anaesthesia (when the child is heavily sedated) is undertaken in a hospital setting. During a general anaesthetic session, the dentist examines thoroughly in the mouth and usually provides a comprehensive treatment including full mouth scaling, fillings and pulling out teeth where necessary. Following a comprehensive treatment under general anaesthesia, the child should go for regular dental check-up for preventive care.
Useful Apps
- My Healthy Smile App for iPhone/iPods
- Leila’s First Visit to the Dentist App for Android
References
- Friedlander AH, Yagiela JA, Paterno VI, Mahler ME. The neuropathology, medical management and dental implications of autism. The Journal of the American Dental Association 2006;137(11):1517-27.
- Nelson TM, Sheller B, Friedman CS, Bernier R. Educational and therapeutic behavioral approaches to providing dental care for patients with Autism Spectrum Disorder. Special Care in Dentistry 2014:n/a-n/a.
- Stein LI, Polido JC, Mailloux Z, Coleman GG, Cermak SA. Oral care and sensory sensitivities in children with autism spectrum disorders. Special Care in Dentistry 2011;31(3):102-10.
- https://www.autismspeaks.org/family-services/tool-kits/dental-tool-kit
| Last Reviewed | : | 11 May 2015 |
| Writer | : | Dr. Eileen Yap Ai Ling |
| Accreditor | : | Dr. Norjehan bt. Yahaya |












