The condition of bleeding gum is not healthy, therefore it shouldn’t be ignored by all. Bleeding gum can be caused by various factors (multifactorial). It can occur at the beginning stages of gum infection like gingivitis, or be a signal of more serious health problems.
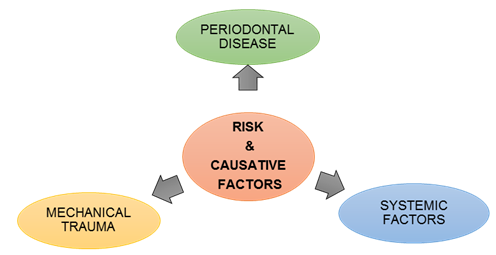
Risks and Causative Factors for Bleeding Gum
Bleeding gum may be associated with various causes and risk factors:
- Bleeding Gum as a Common Sign of Periodontal Disease (Gum Disease)Bleeding gum is one of the important signs of gum inflammation. The most common cause of bleeding gum is poor oral hygiene, which is closely related to periodontal disease. The commonest forms of periodontal disease are gingivitis and periodontitis. In Malaysia, periodontal disease has been shown to be highly prevalent, affecting 94.0% or 14.4 millions of our Malaysian population (NOHSA, 2010).
Dental Plaque and Periodontal Disease
The main cause of bleeding gum is the formation of bacterial plaque on a daily basis at the gum margin and interdental area (between teeth), which is usually caused by poor oral hygiene.
Dental plaque is a film of bacteria which is naturally and constantly forming on all tooth surfaces and at the gum margin. The human saliva contains millions of bacteria, which stick to the tooth surfaces and multiplies quickly to form dental plaque. Researchers has currently defined dental plaque as a diverse community of pathogenic microorganisms found on the tooth surface known as dental biofilm (Marsh, 2004).
If dental plaque is left undisturbed, bacteria can spread into the area below the gum margin inducing a more serious gum problems. The presence of bacterial plaque and its inflammatory-products underneath the gum margins will stimulate the natural body’s defence system targeting the infected area. In response to this, there will be an increased blood supply at the area of infection, forming the signs and symptoms of inflammation such as redness, bleeding and swollen gum. Clinically, this is known as plaque-induced gingivitis (inflammation of gums) where the infection is confined within the gums (Mariotti, 1999).
Dental plaque that is not properly cleaned or removed will start to harden into calculus or tartar within a few days. Calculus is formed when calcium in the saliva combines with dental plaque. In Malaysia, the survey has shown that the presence of calculus is the highest prevalence (41.4%) of all gum condition among the Malaysian adults (NOHSA, 2010).
Plaque retentive factors also may act as a risk factor for bleeding gum, as it may modify or predispose to plaque-induced gingival disease (Blieden, 1999; Ishikawa et. al., 1999). These local factors may include:
 In susceptible individual, prolonged presence of gingivitis may act as a precursor to periodontitis. Pronounced inflammatory response of the gum to bacterial plaque, if without treatment, will result in persistent gum bleeding and further disease progression. The infection will not be confined to the gums only but spread to the other tooth supporting structures such as the alveolar bone.
In susceptible individual, prolonged presence of gingivitis may act as a precursor to periodontitis. Pronounced inflammatory response of the gum to bacterial plaque, if without treatment, will result in persistent gum bleeding and further disease progression. The infection will not be confined to the gums only but spread to the other tooth supporting structures such as the alveolar bone.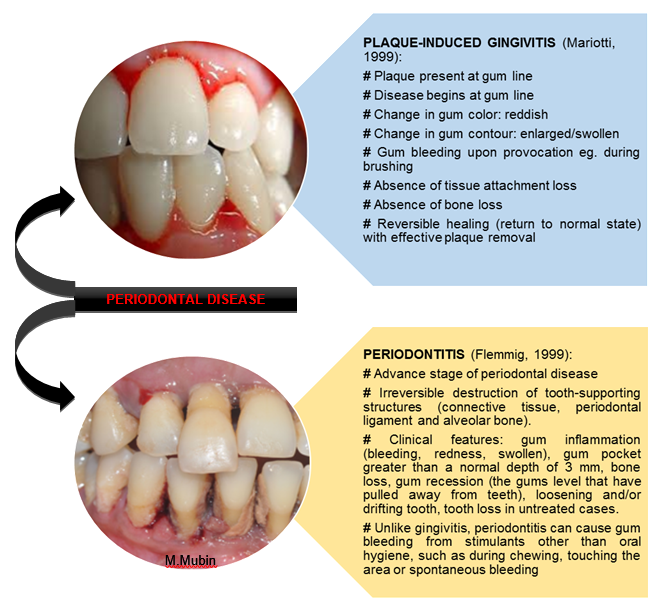 In the advance stage of periodontal disease like periodontitis, the inflammation will extend deep into the tooth supporting structures causing clinical attachment loss, as a result of further destruction of connective tissue and alveolar bone.
In the advance stage of periodontal disease like periodontitis, the inflammation will extend deep into the tooth supporting structures causing clinical attachment loss, as a result of further destruction of connective tissue and alveolar bone.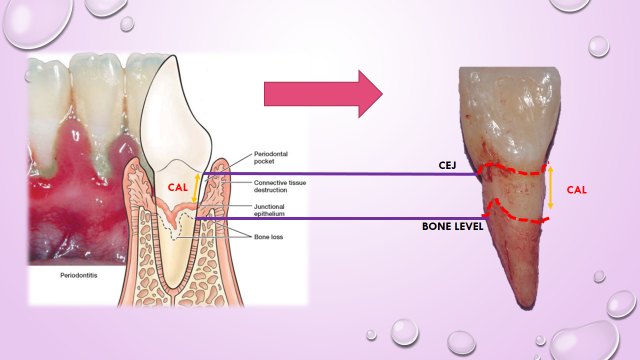 Source: Color Atlas of Dental Hygiene *CAL= clinical attachment loss
Source: Color Atlas of Dental Hygiene *CAL= clinical attachment loss
2. Bleeding Gum Associated with Systemic Factor and Medical Problem (Mariotti, 1999; Caton et. al., 1999; Holmstrup, 1999)
Several systemic condition may be related or manifested by sign of bleeding gum. These include:
- Gingival disease related to viral infections (eg. Herpes simplex and varicella-zoster virus) or fungal infections (eg. Candidiasis), and individual with compromised immune status such as HIV patients
- Hormonal changes: puberty, menstruation or pregnancy.

- Endocrine disease: diabetes mellitus-associated periodontal disease.
- Haematological disorders: leukemia, idiopathic thrombocytopenic purpura.
- Malnutrition: scurvy, ascorbic acid-deficiency gingivitis, vitamin K deficiency.
- Medications: oral contraceptive-associated gingivitis, drug-induced gingival enlargement (e.g phenytoin, nifedipine or cyclosporine medications) in which the gingival overgrowth will promote the accumulation of dental plaque and calculus within the gum pockets.
- Mechanical Trauma to the Gum (Holmstrup, 1999):Bleeding gum can also be caused by physical injury to the gum tissue. The injury may include:
- Improper oral hygiene procedures: incorrect brushing or flossing techniques, greater brushing/flossing force
- Improper selection of oral hygiene tools: hard-bristle toothbrush, incorrect size of interdental brush, improper usage of toothpick
- Impaction or injuries by foreign objects (e.g. fishbone, toothbrush bristle) that cause gum infection and inflammation
- Poorly contoured restorations, dentures or other dental appliances
- Self-inflicted gum injury: chronic habits of fingernail biting, digit sucking or object sucking
Treatment
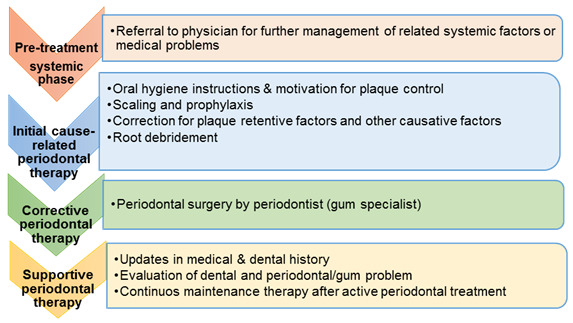
Once you noticed your gum bleeds easily, then you need to see your dentist immediately to work out the possible causes, either you have periodontal disease or any other related medical problems. Early detection is very important because depending on its causative factor, bleeding gum may be something that can easily be reversed by good oral hygiene practice. However, if severe infection is the cause, then more complex periodontal treatments will be needed.
Periodontal treatments (gum treatment) will be provided based on the type of cases and its severity. The phases of treatment may include:
In the pre-treatment phase, once the medical history is evaluated, referral to physician for further management of related medical problem is required for further stabilisation of the systemic factor.
Proper plaque control that includes effective tooth brushing and thorough interdental cleaning are particularly important for removal of all plaque and food debris responsible for gum inflammation. However, once the calculus (tartar) has formed due to the long existing of undisturbed plaque, it can only be removed by professional scaling and prophylaxis in dental clinic.
Apart from that, cause-related therapy is significantly important for correction of plaque retentive factors as well as any other causes that are related with mechanical injuries to the gum or factors that causing gum inflammation.
In case of gingivitis, the condition is still reversible with daily effective oral hygiene at home and by professional cleaning, without the need of complex periodontal procedures.
However, in advanced cases like periodontitis, other than scaling and root debridement, the subsequent periodontal surgical procedures can be provided in corrective phase based on the type and severity of the cases.
Once the gum condition is stabilised, the follow-up visit under maintenance phase is recommended.
Prevention
It is very important that you keep up a good routine at home to keep your teeth and gum healthy. For that, our recommendations of preventive measures include:
- Regular tooth brushing at least twice a day, for removal of plaque and food debris between the teeth. These will help to keep your teeth and gum healthy. The use of soft bristle toothbrush with correct brushing technique can prevent injuries to your gum. If you notice any gum bleeding while brushing, this means your gum is not healthy and you need to brush and floss more often and more thoroughly, or you may need your teeth professionally cleaned. You may ask your dentist or periodontist (gum specialist) for further advice on proper oral hygiene techniques and tools.
- Interdental cleaning using dental floss with proper flossing method is particularly required at the teeth contact points and at the narrow interdental area (between the teeth) for at least once daily. This is because the regular toothbrushes will not clean interdental areas effectively as their filaments are not able to reach deep enough areas between the teeth. For those with gaps between their teeth, it is recommended to use interdental brushes to clean the larger interdental spaces.
- The use of antiseptic mouth rinse as an adjunct to mechanical cleaning may help to remove excess bacteria in the area that are less accessible to brushing or flossing.
- Eat a well-balanced diet and limit the snacking habits for healthy teeth and gums. Reducing the quantity and frequency of sugar consumption is good as sugar can promote the growth of dental plaque.
- Smoking habit will harm nearly every organ of the body. Smoking cessation will enhance your body immune system and lowers your risk for smoking-related diseases including gum disease (periodontitis).
- Watch out for any warning signs and symptoms of gum disease such as gum redness, bleeding, changes in gum shape, gum recession, presence of pus, loose teeth, teeth that have changed its position and bad breath. Early detection and treatment may prevent further disease progression.
- Visit your dentist regularly (at least twice a year) for consultation regarding your oral health condition, routine oral examination and dental / gum treatment. This is very important for early detection of any possible problems you may have and to ensure your teeth and gum are in a healthy state. Further diagnosis of your gum problem also can only be confirmed once you visit your dentist or periodontist (gum specialist). For whatever causes, it is best for you to get treatment early, for a better prognosis.
Preventive measure is a better way of helping you to keep a healthy mouth. The earlier you prevent or manage your gum problems, the higher chances that you are able to keep your teeth for life. Prevention is better than cure.
References
- American Academy of Periodontology (2000). Parameter on Plaque-Induced Gingivitis. J Periodontol, 71(5), 851-852.
- Blieden, T. M. (1999). Tooth-related issues. Annals of Periodontology, 4(1), 91-96
- Caton, J. G., Williams, R., Zappa, U., Claffey, N., Greenwell, H., Mahanonda, R., Mariotti, A., Zackin, J. (1999). Consensus report: Dental plaque-induced gingival disease. Annals of Periodontology, 4(1), 18-19
- Flemmig, T. F. (1999). Periodontitis. Annals of Periodontology, 4(1), 32-37
- Holmstrup, P. (1999). Non-plaque-induced gingival lesions. Annals of Periodontology, 4(1), 20-29
- Ishikawa, I., McGuire, M. K., Mealey, B., Blieden, T. M., Douglass, G. L., Hallmon, W. W., Nevins, M., Polson, A. M.,Prato, G. P. P., Schallhorn, R. G., Wennstrom, J. L. (1999). Consensus report: Localized tooth-related factors that modify or predispose to plaque-induced gingival disease and periodonttis. Annals of Periodontology, 4(1), 97
- Mariotti, A. (1999). Dental plaque-induced gingival disease. Annals of Periodontology, 4(1), 7-17
- Marsh, P. D. (2004). Dental plaque as a microbial biofilm. Caries Res, 38, 204–211
- Oral Health Division, MOH. (2010). National oral health survey of adults 2010 (NOHSA 2010). Kuala Lumpur: Oral Health Division, Ministry of Health Malaysia.
- Wolf H. F, Hassell, T. M., (2006). Color Atlas of Dental Hygiene. New York: Thieme
| Last Reviewed | : | 25 August 2015 |
| Writer | : | Dr. Marina bt. Mubin |
| Accreditor | : | Dr. Yuhaniz bt. Ahmad Yaziz |