Introduction
Brain tumour is an abnormal and uncontrolled growth of cells in the brain. Brain tumours can be divided into:
- Primary brain tumour – tumour originates from the brain
- Secondary brain tumour – tumour spread to the brain, from cancer at other part of the body, such as lung, breast, prostate, kidney
Primary brain tumour are further divided to:
- Benign – slow growing tumours, do not spread to other parts of the body and do not invade surrounding tissues. It is also less likely to come back after complete removal
- Malignant – fast growing tumour and may invade surrounding tissues. They rarely spread to other parts of body outside brain. It is more likely to come back even after complete removal.
Both of them can grow bigger and cause compression on structures of the brain such as the eyes, causing blindness.
Primary brain tumours are rare. Malignant brain tumour is even rarer – around 2% of all cancers in adults. In UK, the overall annual incidence of all brain tumours is 7 per 100,000 populations. In USA, the yearly incidence of all brain tumours is 46 per 100,000 and only 15 per 100,000 of them are primary brain tumours.
Males are more likely to be diagnosed with brain tumours than females (ratio: 1.5:1)
Risk factors
There are several factors that slightly increase the risk of developing a brain tumour.
- Age – brain tumours are more common in older people
- Radiation exposure (radiotherapy)
- Weakened immune system
Other possible risk factors that have been postulated are mobile phones, power lines and certain viruses. However, there is no evidence to support them as risk for tumours. Tobacco, alcohol, hair dyes, pesticides, air pollution, aspartame diet and head trauma are also not associated with higher risk of tumour.
Small number of brain tumours is inherited – such as Neurofibromatosis, Tuberous Sclerosis, Li Fraumeni syndrome, von Hippel Lindau syndrome.
Symptoms and signs
Most common symptoms are headaches and fits (seizures). Headaches (half of all patients) are usually generalised and worse in the morning but wear off as the day goes on. This is due to increased pressure in the skull. The headaches are also usually associated with vomiting. Seizures occur at presentation in 15-95% of patients with brain tumour, and are typically focal in type.
Other symptoms include:
- Feeling sick
- Blurring of vision
- Drowsiness
- Changes in personality, memory or mental status
- Weakness of one side of body
- Numbness of one side of body
- Difficulty in speaking or hearing
- Difficulty in smelling or tasting
Unsteadiness in standing and walking
Investigations
Brain CT (Computer Tomography) scan
- Using x-rays to make a three-dimensional picture of the brain to show position of the tumour
Brain MRI (Magnetic Resonance Imaging)
- Using magnets and radiowaves to produce images of the brain.
- Able to give a more detail picture of the brain tumour
EEG (Electroencephalogram)
- A non-invasive test that records activities of the brain
- Important in patients presenting with seizures.
Lumbar puncture
- Getting a sample of the cerebrospinal fluid which is taken from the lower back
- Usually not done if there are signs of high pressure in the skull (based on CT scan/ MRI scan and clinical features)
Biopsy (surgery)
- Removal of a small piece of the tumour for exact diagnosis of type of tumour
Types of brain tumours
Glioma
- Half of all primary tumours
- 3 main types – astrocytoma, ependymoma, oligodendroglioma
Acoustic neuroma
- Slow growing tumour in the nerve that runs from the ears to the brain
- Benign tumour and do not spread
- Most common presentation – loss of hearing in one ear
- More often in older people
Astrocytomas
- Commonest type of glioma
- Develop from cells called astrocytes (cells that support the nerve cells)
- Can be fast or slow growing
- Can be focal (distinct border between tumour and normal cells) or diffuse (no clear border)
- Anaplastic astrocytoma (Grade 3 astrocytoma) and glioblastoma multiforme (Grade 4 astrocytoma)
- commonest malignant brain tumours in adults
- may spread to other parts of brain
Craniopharyngiomas
- Tumours tend to grow near base of the brain, just above the pituitary gland.
- Most often in children, teenagers and young adults
- Can cause altered vision and hormonal disturbances
- Benign tumour and do not spread
Ependymomas
- 5% of all brain tumours
- Develop from cells called ependymal cells (cells that line the fluid-filled areas of brain and spinal cord)
- Mainly in young adults
- Can be high or low grade
Hemangioblastomas
- 2% of all brain tumours
- Tumours grow from blood vessel cells
- Very slow growing and do not spread
Lymphomas (Primary cerebral lymphoma)
- It is a cancer of the lymphatic system
- Usually occurs in people with poor immunity system (organ transplant or AIDS patient)
Meningioma
- Occurs in around 25% of all brain tumour
- More common in older people and in women
- Usually benign
- Most often found in forebrain or hindbrain
Oligodendroglioma
- 5% of all brain tumours
- Derived from cells called oligodendrocytes (cells that make the nerve covering – myelin)
- Most often in forebrain
- Can be fast or slow growing
Pineal region tumours
- Rare (around 1% of all brain tumours)
- A gland that produce hormone melatonin
Pituitary tumours
- Around 1% of all brain tumours
- More common in older people
- Usually benign, slow growing and do not spread
- Causes excessive hormone production
Primitive Neuroectodermal tumours
- Develop from cells that are left over from the earliest development of body
- Usually harmless but can be cancerous
- Most common type is medullablastoma
Spinal cord tumours
- 20% of central nervous system tumours
- Commonest types are meningioma and neurofibrom
Management
This must be done by a multidisciplinary team – neurologist, neurosurgeon and clinical oncologist
- to determine the best management for the patients
- choice of treatment is dependent on type of tumour
Treatment available include:
- Surgery
- either via craniotomy or stereotactic
- either complete resection or debulking/ partial resection (if cannot remove whole tumour)
- Chemotherapy
- uses medicine to destroy cancer cells
- can be used in combination with radiotherapy
- Radiotherapy
- using high-energy rays (radiation) to destroy cancer cells while doing little harm to surrounding normal cells
- often used after surgery or given in combination with chemotherapy (high grade tumours)
- to treat secondary brain tumours
- to treat primary brain tumours that can’t be removed or has recur
- Supportive treatment
- antiepileptic drugs – to treat any seizures
- steroids (dexamethasone) – to control any problems caused by secondary brain tumours (control brain swelling)
Outcome
Outcome of the brain tumours is dependent on
- Type of tumour
- Grade of the tumour
Overall, for all types of adult brain tumours, 30% will live for at least a year. 14% live for more than 5 years after diagnosis. Just less than 10% diagnosed live for more than 10 years after diagnosis.
The outcome is better for younger patients.
Fast growing tumours are more likely to recur after treatment.
Sometimes, the tumour cannot be removed completely due to its location near to vital organs in the brain.
- This can lead to higher risk of recurrence
References
- McKinney PA. Brain tumours: Incidence, survival and aetiology. Journal of Neurology Neurosurgery Psychiatry 2004;75:ii12-ii17
- Brain tumour information centre: Cancerbackup. www.cancerbackup.org.uk/Cancertype/Brain
- Brain tumours: Cancer Research UK: Cancerhelp UK.www.cancerhelp.org.uk/help
- BUPA: Brain tumours. hcd2.bupa.co.uk/fact_sheets/mosby…/brain_tumours.html
- DeAngelis LM. Brain tumours. New England Journal of Medicine 2001:344:114-123
- Behin A, Khe HX, Carpenter AF, Delattre JY. Primary brain tumours in adults. Lancet Journal 2003:361:323-331
Figures
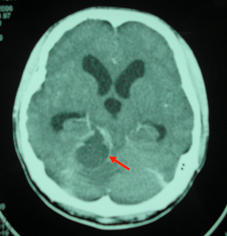
Figure 1: CT scan brain showing a cerebellar tumour (red arrow) with complications of obstructive hydrocephalus
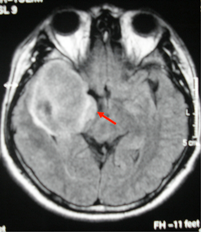
Figure 2: MRI brain showing a temporal lobe tumour (red arrow)
| Last reviewed | : | 20 June 2014 |
| Writer | : | Dr. Mak Choon Soon |
| Accreditor | : | Dato’ Dr. Hj. Md Hanip b. Rafia |
| Reviewer | : | Dr. Mohd Sufian b. Adenan |







