What is normal weight?
Children gain weight as they grow. Their ideal weight increase as their height and age increase.
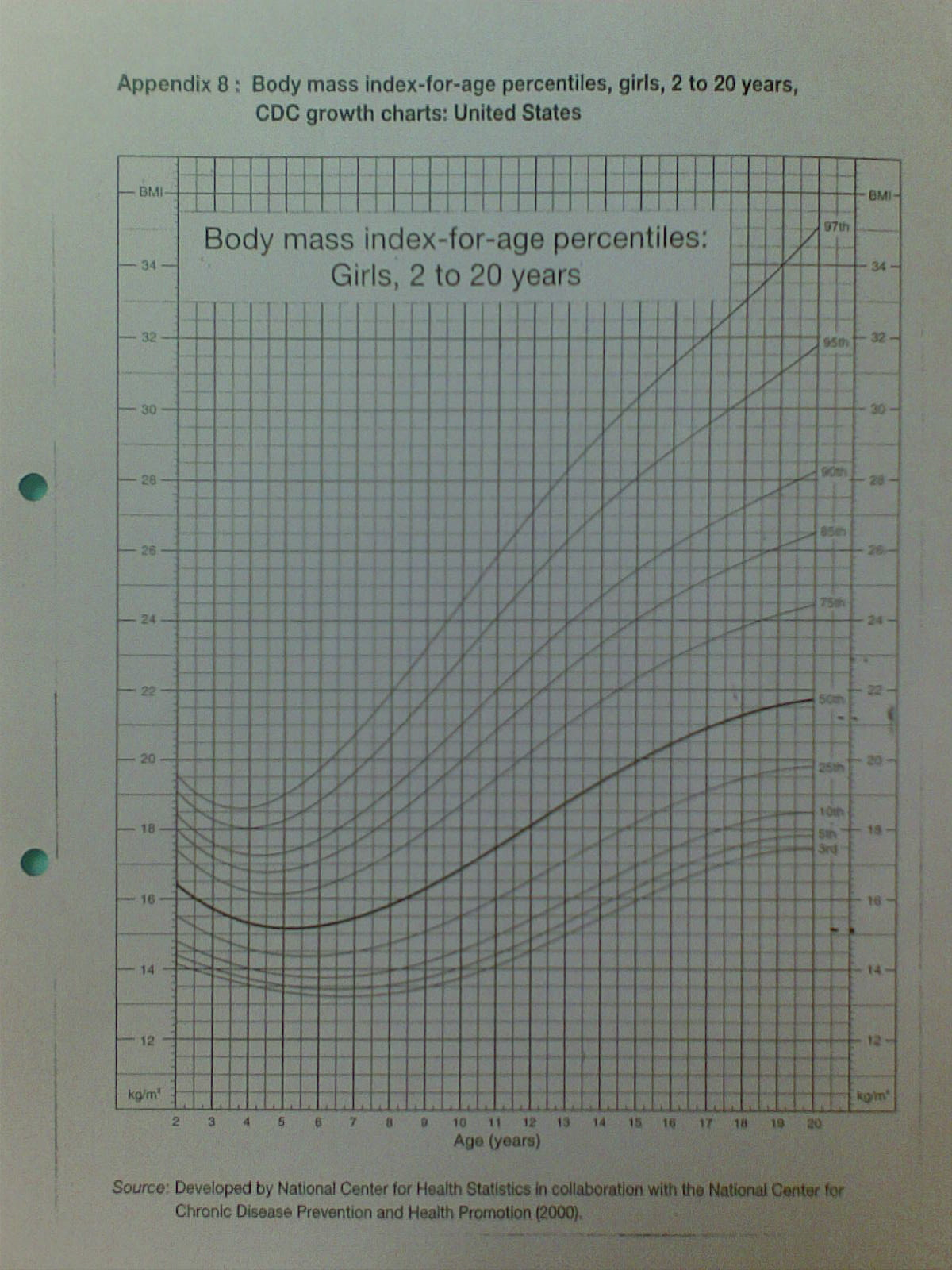
Therefore, you need to refer to the body mass index (BMI) chart in order to check if your child is having normal weight or overweight. (Refer figure 1).
What is overweight?
World Health Organization defined obesity using body mass index (refer to figure 1).
What is obesity?
- BMI = weight (kg) / height² (m²)
- Overweight : BMI at or above 85th percentile (Refer to Figure 1) for children and teens of same age
- Obesity: BMI at or above 95th percentile for children and teens of same age
- Severe obesity: BMI above 99th percentile
How common is overweight problem in Malaysia?
Overweight / obesity rate in children and adolescents has increased over the years. Up to 30% of Malaysian children were found to be overweight / obese.
What causes overweight/obesity?
The main cause of obesity in children is exogenous obesity, which is due to external factors.
Though body fatness is heritable, the environmental factors play a more important role in body weight because we can modify our environment.
Less than 1% of childhood obesity referred to hospital is due to endocrine and genetic disease.
Regardless of the cause, obesity is due to calorie consumption in excess of calorie burnt.
Weight Gain = Calories Consumed > Calories Burned
Health risks of overweight / obese children
Overweight/obese children are exposed to the following health risks;
- Type 2 diabetes mellitus: This can occur in patients as young as 8 years old.
- High Blood Pressure – The risk of high blood pressure increases as the severity of obesity increases. High blood pressure over a long duration strains the heart.
- Liver Problems – Fatty liver disease (nonalcoholic steatohepatitis or NASH) is common among obese children and can lead to liver failure (cirrhosis).
- Obstructive sleep apnea: This is a potentially life-threatening breathing disorder caused by upper airway obstruction in obese children. Affected children have snoring and brief interruptions of breathing during sleep. It can lead to heart failure without intervention.
- Gallstones – Obese children have higher risk of getting gallstone diseases.
- Joint damage – Carrying extra body weight over a long duration can lead to damage in the weight bearing joints, such as the knee and ankle joints.
- Metabolic syndrome and risk of heart disease – Metabolic syndrome is a condition characterized by combinations of abnormal lipids, high blood pressure, abnormal glucose level and obesity. About 30-40% of overweight/obese children fulfills the criteria of metabolic syndrome, and has significant higher risk of heart problem in later life.
- Heart Disease – Atherosclerosis (stiffening of the blood vessels) is the most common cause of heart disease. This can occur as early as during childhood and adolescents, especially in those with metabolic syndrome.
- Menstrual Problems – Overweight girls tend to enter puberty earlier. In later life, there is higher risk of uterine fibroids and menstrual irregularities.
- Persistent overweight as adults: Overweight children tend to grow into overweight adults. Almost half of overweight adults were overweight as children.
- Depression – Being overweight can lead to self-esteem problems that lead to depression. Depression is associated with poor sleep, inactivity, and depressive eating, which can aggravate weight gain.
How to deal with an overweight/obese child?
Obese adults and adolescents who have completed growth should aim for weight loss. Unlike adults, obese children should maintain their weight as they grow (grow into a healthy body weight). This can reverse the negative effects of obesity.
Health risks associated with obesity respond well to good dietary practice and physical activity.
- Regular physical activity, at least 1 hour a day helps to control weight, reduces your health risks of obesity, and increases bone/muscle strength. Children should get involved in variety of activities they enjoy, such as team sports, swimming, yoga, riding a bike, taking a dance class or an evening walk after dinner. A good exercise program does not need to be strenuous. It should include stretching to promote flexibility and strength training to build muscle. For preschool-aged children, outdoor play is particularly helpful.
- Parents should show interest and support in their children’s activities. Set an attainable goal that fits with your child’s physical ability and preferences. Keep a chart to track your child’s progress and praise your child when goal is achieved. Show a good example and make the physical activity a family activity.
- Limit sedentary behaviors (videos or movies, video games, internet-based activities) aside from schoolwork, to less than 2 hours a day. Use staircase rather than elevator or lift.
- Encourage your child to eat 5 servings of fruits and vegetables a day. Add some fun to your child’s plate by giving healthy food with various colours, such as tomato, broccoli, corn, carrots, potato and green peas. Encourage fresh fruits such as watermelon, star fruit, orange rather than juice.
- Avoid skipping meals that can lead to eating too much at the next meal.
- Main meals should be taken at home, together with the family. Avoid watching television during mealtime.
- No television allowed in a child’s bedroom.
When to refer to Paediatric Endocrinologist?
Obese children or adolescents should be referred to a Paediatric Endocrinologist when:
- Overweight/obesity with comorbidities.
- All children with type 2 diabetes mellitus.
* Obese children or adolescents with depression should be referred to Psychologist/ Psychiatrist.
When and how to investigate for comorbidities of obesity?
- Oral glucose tolerance test (ingestion of glucose and blood glucose level checked at 0 hour and 2 hours) may be indicated in selected cases to look for diabetes mellitus. This is indicated for overweight/obese children who are/have:
- Older than 10 years old (earlier if puberty occurs before 10 years old).
- At the onset of puberty.
- 2 or more risk factors (Family history of type 2 diabetes in a first or second degree relative; Ethnic background of African-American, Hispanic, American Indian, Asian, or Pacific Islander origin.
- Presence of acanthosis nigricans (darkening and thickening of skin at the neck area), polycystic ovary syndrome, high blood pressure, and lipid disorders.
- Other investigations as indicated:
- Blood cholesterol level.
- Liver function test.
- Ultrasound liver if fatty liver is suspected.
Is medicine available for weight reduction in children?
The use of weight reducing medication is very limited in children due to the concern of adverse reactions in growing children. However, it may be considered for short-term use in selected cases under close medical supervision.
How to prevent childhood obesity?
From today onwards, adopt a healthy lifestyle by staying active and eating a healthy diet.
Educate your children that maintain a healthy lifestyle will help improve their ability to learn at school and keep their body strong.
Work with your children’s school to create a healthy and active environment.
 |
|
Figure 1: BMI charts for girls aged 2 to 20 years old |
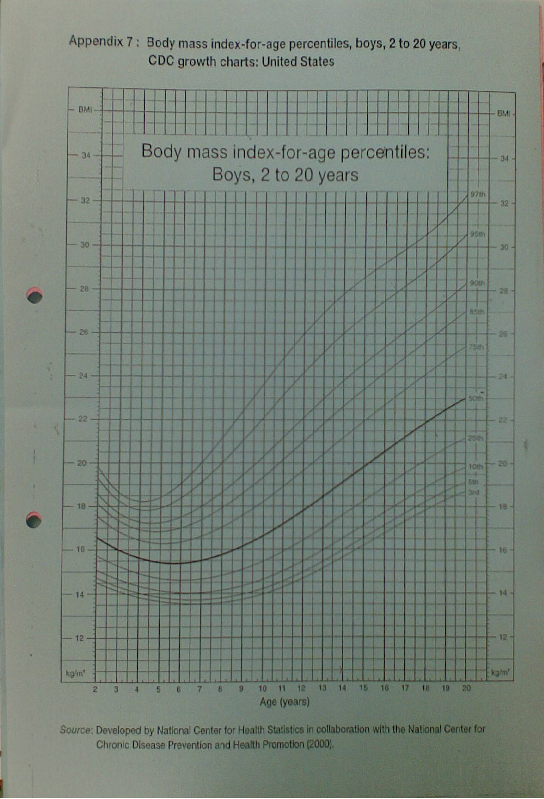 |
| Figure 2: BMI charts for boys aged 2 to 20 years old |
Reference :
- Tracking of overweight status from childhood to young adulthood: the Bogalusa Heart Study Deshmukh-Taskar P et al, European Journal of Clinical Nutrition (2006) 60, 48–57. doi:10.1038/sj.ejcn.1602266 published online 31 August 2005
- Risk of metabolic syndrome among children living in metropolitan Kuala Lumpur: A case control study, Bee S Wee1,2, Bee K Poh1*, Awang Bulgiba3, Mohd N Ismail1, Abdul T Ruzita1 and Andrew P Hills4, BMC Public Health 2011, 11:333
- Evaluation and management of childhood and adolescent obesity. Singhal V, Schwenk WF, Kumar S.Singhal V. Mayo Clin Proc. 2007 Oct;82(10):1258-64.
- Consequences of Childhood Obesity, Lee YS et al, Ann Acad Med Singapore 2009;38:75-81
| Last Reviewed | : | 28 August 2020 |
| Writer | : | Dr. Janet Hong Yeow Hua |
| Reviewer | : | Dr. Zainab bt. Kusiar |







