“Early” cord clamping is generally carried out in the first 60 seconds after birth (generally within the first 15–30 seconds), whereas “delayed” umbilical cord clamping is carried out more than 1 minute after the birth or when cord pulsation has ceased. Cord clamping means “the tying and cutting of the navel string”.
Incidence
The incidence is low as the practice of delayed cord clamping is new to modern obstetrics practice.
Advantages
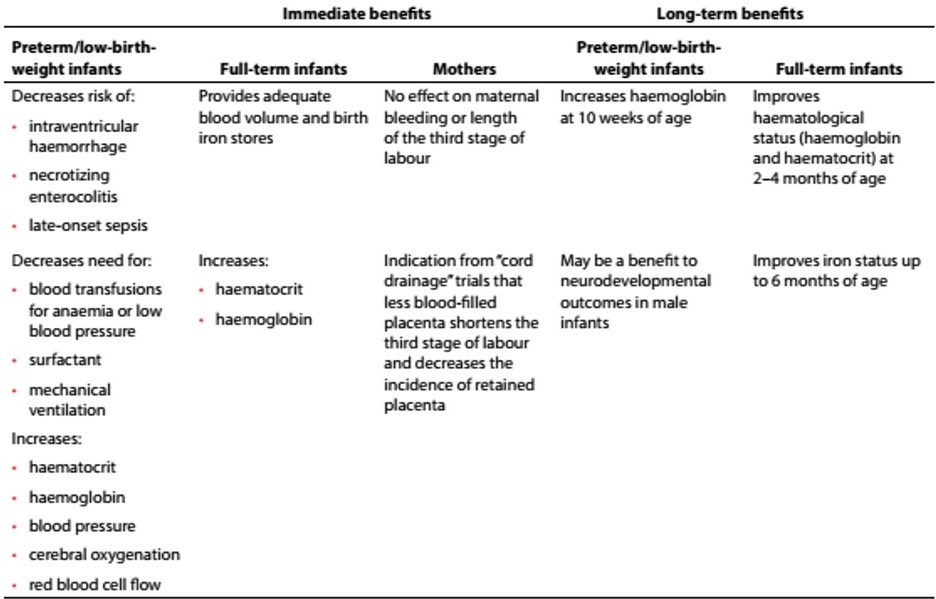
There is growing evidence that delayed cord clamping is beneficial and can improve the infant’s iron status for up to 6 months after birth. For the first few minutes after birth, there is still circulation from the placenta to the infant. Waiting to clamp the umbilical cord for 2–3 min, or until cord pulsations cease, allows a physiological transfer of placental blood to the infant (the process referred to as “placental transfusion”), the majority of which occurs within 3 min. (see table 1).
Table 1 : Summary of immediate and long-term benefits of delayed umbilical cord clamping for infants (term, preterm/low birth weight) and mothers from individual studies
This guideline compiles current WHO recommendations on umbilical cord clamping for maternal and infant health outcomes, in preterm and term births
This placental transfusion provides sufficient iron reserves for the first 6–8 months of life, preventing or delaying the development of iron deficiency until other interventions –such as the use of iron-fortified foods– can be implemented. Iron deficiency in the first few months is associated with neurodevelopmental delay.
Disadvantages
- If there is a need for immediate resuscitation of the baby: The timing of umbilical cord clamping is also relevant to neonatal resuscitation practices. About 25% of all neonatal deaths globally are caused by birth asphyxia, defined simply as the failure to initiate and sustain breathing at birth. Effective resuscitation at birth can prevent a large proportion of these deaths. In many settings, immediate clamping and cutting of the umbilical cord is needed in order to begin resuscitation protocols for the infant, largely due to the location of resuscitation equipment in the delivery
room that requires transfer of the neonate. Whether resuscitation with the cord intact is beneficial is an unanswered question, though recent research has shown that it is a feasible practice, at least in some settings. - Postpartum hemorrhage as the outcome in relation to umbilical cord clamping time: There were no significant differences in the rates of severe postpartum hemorrhage (>1000 mL) or postpartum hemorrhage (>500 mL) between groups with early or delayed umbilical cord clamping. In addition, no significant effect of umbilical cord clamping time was observed in the trials but more trials are needed to address this issue.
- Jaundice may be more common after deferred cord clamping but this management is likely to be beneficial as long as phototherapy for jaundice is available.
For term births, while the cord is intact the baby can be placed on the mother’s abdomen or chest following a vaginal birth without influencing the volume of placental transfusion. Owing to the influence of gravity on placental transfusion, sensible advice is that while the cord is intact the baby should not be lifted higher than this.
The timing of cord clamping should be routinely recorded in medical notes.
The administration of intramuscular uterotonic drugs (e.g. oxytocin) before cord clamping is unlikely to have a substantive effect on placental transfusion.
For preterm births the evidence is less clear than for term births, although data from the trials suggest potential benefit by deferred rather than immediate cord clamping.
Cord milking is an alternative to deferred cord clamping for preterm births, but requires further evaluation of its benefits and risks before entering routine practice.
Recommendation of WHO:
- In newly born term or preterm babies who do not require resuscitation, the cord should
not be clamped earlier than 1 min after birth. - When newly born term or preterm babies require resuscitation, the cord should be
clamped and cut to allow effective ventilation to be performed. - Newly born babies who do not breathe spontaneously after thorough drying should be stimulated by rubbing the back 2–3 times before clamping the cord and initiating resuscitation.
- Late cord clamping (performed approximately 1–3 min after birth) is recommended for all births, while initiating simultaneous essential neonatal care.
- Early umbilical cord clamping (less than 1 min after birth) is not recommended unless the neonate is asphyxiated (unable to breath) and needs to be moved immediately for resuscitation.
References
- The royal college of Obstetricians and Gynecologists UK,
| Last Reviewed | : | 23 August 2019 |
| Writer | : | Dr. Hj. Mohamed Hatta b. Mohamed Tarmizi |
| Accreditor | : | Dr. Haris Njoo Suharjono |
| Reviewer | : | Dr. Rafaie bin Amin |







