Bruises occur as a result of blood leaking out of the blood vessels within the skin. Bruises are common in children when they go about their normal activities. Children fall while playing, run into each other or bump into furniture. Bruises that need worrying are those which occur spontaneously or that are out of proportion to the injury.
Abnormal bleeding can be caused by:
- disorder of blood vessels (vascular disorders)
- quantitative or qualititative problems of blood cells called platelets or
- defective blood coagulation process
Platelets are cells produced by the bone marrow. Following blood vessel injury, platelets will stick to the exposed blood vessel lining (subendothelial connective tissue) to form a mechanical plug. Fibrin enmeshes the platelet aggregates at the site of vascular injury and convert the rather unstable platelet plug to form definitive stable hemostatic plug. The production of fibrin involves a biological amplification system called the coagulation pathway. The operation of this system requires local concentration of circulating coagulation factors at the site of injury. At present there are14 known coagulation factors and a defect in any of these factors may disturb the coagulation system and cause bleeding problems. There are many diseases that can cause easy bruising in children, some are more common than others. The common ones are:
- Vascular Disorders (disorder of blood vessels)
Vascular disorders are conditions characterized by easy bruising and spontaneous bleeding from small vessels. The underlying abnormality is either in the vessels themselves or in the connective tissue around the blood vessels. The bleeding is usually not severe. Frequently the bleeding is in the skin causing bruises or small pinpoint non-itchy red dots called petechiae or both.
Petechiae occur when very small blood vessels called capillaries bleed under the skin. In some there is also bleeding from mucosa (commonly the lining of the oral cavity).
- Scurvy
In an otherwise normal child, vitamin C deficiency can cause bleeding into the mucosa, bruising and petechiae. This condition is called Scurvy and is due to defective intracellular substance of blood vessels. - Haemangioma
Haemangiomas are abnormal vascular growth which develop in the skin, mucous membranes and internal organs. They usually appear in infancy, can bleed with minor trauma or by themselves. These abnormal blood vessels are usually tortuous and can cause sluggish blood flow. Due to this, platelets can be trapped and in turn cause bleeding due to it’s lack in the general blood circulation. Consumption of platelets in haemangiomas is called “Kassabach Merrit Syndrome”.
- Scurvy
- A. Quantitative Platelet Problem
Two common conditions in children are Primary Immune Thrombocytopenic Purpura (ITP) and Acute Leukaemia.a. Example of increased pIatelet destruction : Immune Thrombocytopenic Purpura
Primary ITP in children usually occurs between the ages of 2 and 6 years of age, and. Primary ITP usually occur after a viral illness. Antibodies are formed and act againts platelets. Although the amount of platelets produced by the bone marrow is adequate, the levels in the blood are lower than normal, so bruising with minimal or no injury occurs. Platelets that stick together at the site of an injury is insufficient to stop bleeding. In addition to bruising, ITP causes petechiae and bleeds. In 80% of children, primary ITP lasts six months or less ( Acute ITP) and then spontaneously disappears. Primary ITP that last for more than 6 months is termed Chronic ITP. It can persist for years before spontaneously recovering.
Plaletet transfusion will not help to increase the platelet count as antibodies in the child will act against the transfused platelets. Steroids or intravenous immunoglobulins may increase the platelet count in severe bleeding conditions.
b. Examples of decreased platelet production: Acute Leukaemia
Acute Leukemia is the most common type of childhood cancer. It affects the production of blood cells in the bone marrow. Immature cells grow out of control, crowding out normal production of white and red blood cells and platelets. Leukemia normally occurs in children between 2 and 5 years old but can affect children of any age. Boys are slightly more likely to develop leukemia than girls.
In addition to bruising, fatigue, fever and shortness of breath often occurs in children with leukemia. There are several kinds of childhood leukemia, with acute lymphoblastic leukemia or ALL, comprising 80 percent of cases. Leukemia is not inherited and the causes are often unknown, although children with certain genetic abnormalities such as Down syndrome are more likely to develop it.
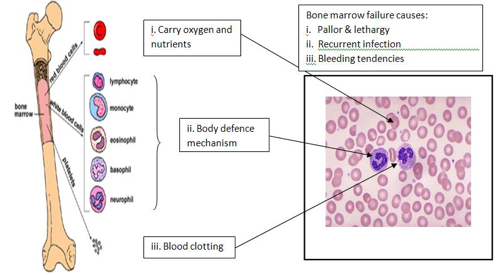
Figure : Blood Cells produced by the bone marrowThe same mechanism of bleeding tendencies occur in Aplastic Anaemia where the bone marrow fails to produce platelets, white and red cells.
- B. Qualitative Platelet ProblemDisorders of platelet function are usually suspected when a person has skin and mucosal haemorrhage despite a normal blood count. They may be hereditary or acquired. Hereditary disorders are rare and among these are:
- Glanzmann’s disease where there is a failure of primary platelet aggregation
- Bernard-Soulier syndrome where the pletelets are larger than normal, have a deficiency of surface glycocprotein and fail to adhere to the wall of blood vessels.
- Von Willebrand disease. It is the is the most common inherited bleeding disorder. The Von Willebrand factor helps platelets clump together and stop bleeding. In this disease there is defective platelet adhesion as well as Factor VIII deficiency. This disease is usually mild, affects males and females equally.
Platetet dysfunction may also be acquired. Many drugs and herbs can cause platelet dysfunction. Examples of drugs include aspirin and dypiridamole. It can also be due to underlying conditions such as renal failure or myeloproliferative disease.
- Problems in Coagulation Process
Hemophilia
There are two types of hemophilia, an inherited clotting disorder, Hemophilia A (Factor VIII deficiency), Haemophilia B or Christmas Disease (Factor IX deficiency) and Von Willebrand disease (as mentioned above). Nearly all children born with hemophilia are boys as the inheritance is sex linked. Females usually are not affected but become carriers. Eighty to 85% of all haemophilia patients have hemophilia A and 10 to 15% have haemophilia B. In hemophilia A, factor VIII level is reduced, and in hemophilia B, factor IX level is reduced. Clotting factors help platelets clump together at the site of injury to stop bleeding.
The Bleeding in hemophilia can range from being mild to severe depending on the level of affected coagulation factors. Seven out of 10 children have the severe form in which only 1% of the normal amount of clotting factor is in the blood. Many children with hemophilia receive regular injections of clotting factor, since bleeding into the joints and other areas of the body that may not be immediately noticed can be extremely dangerous.
Other inherited coagulation factors i.e. Factors XI – XIII are very rare. Acquired deficiency of Factors II, VII, IX and X can be due to Vitamin K deficiency resulting from liver or pancreatic disease or small bowel disease.
| Last reviewed | : | 20 June 2014 |
| Content Writer | : | Dr. Mahfuzah Mohamed |
| Accreditor | : | Dr. Eni Juraidah bt. Abdul Rahman |
| Reviewer | : | Dr. Mahfuzah Mohamed |







