Asthma is a disorder caused by inflammation in the airways (called bronchi) that lead to the lungs. This inflammation causes airways to tighten and narrow, which blocks air from flowing freely into the lungs, making it hard to breathe. Symptoms include wheezing, breathlessness, chest tightness, and cough, particularly at night or after exercise/activity. The inflammation may be completely or partially reversed with or without medicines. The inflammation of the airways makes them very sensitive, resulting in spasm of the airways that tend to narrow, particularly when the lungs are exposed to viral infection, allergens, cold air, exposure to smoke, and exercise. Thus the constriction of the airways results in a reduction in the amount of air going into lungs, making it hard to breathe. Things that trigger asthma differ from person to person. Some common triggering factors for asthma are exercise, allergies, viral infections, and smoke. When a person with asthma is exposed to a triggering factor, their sensitive airways become inflamed, swell up, and fill with mucus. In addition, the muscles lining the swollen airways tighten and constrict, making them even more narrowed. So an asthma flare is caused by three important changes in the airways that make breathing more difficult:
- Inflammation of the airways
- Excess mucus that results in congestion and mucus “plugs” that get caught in the narrowed airways
- Narrowed airways or broncho constriction (bands of muscle lining the airways tighten up)
The tendency to develop asthma is often inherited; in other words, asthma can be more common in certain families. There is also an opinion that said, asthma is the most common chronic disease among children, especially children who have a low birth weight, exposure to tobacco smoke, black, and grew up in a poor family environment. Normally, these symptoms first occurred at age 5 years, generally it starts with frequent episodes of wheezing with respiratory infections. Additional risk factors for children, including those with allergies such as eczema, or parents who also have asthma. Boys are said to have a much higher risk of having asthma than girls. However, this situation will change as they grow. The hypothesis the researchers argue is that the size of the airway in boys is smaller than in girls.
| Respiratory System |
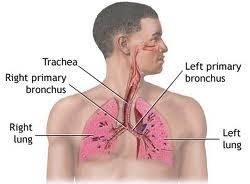 |
|
Source: https://www.nlm.nih.gov/medlineplus/ency/imagepages/9248.htm |
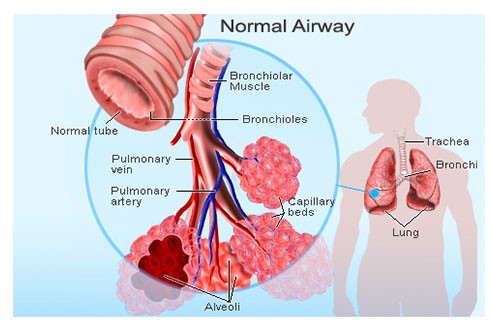 |
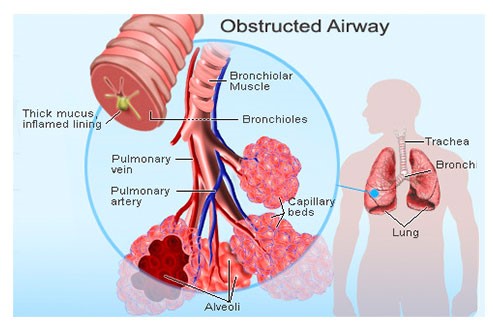 |
Source: http://www.medicinenet.com/asthma_pictures_slideshow/article.htm
Common childhood asthma signs and symptoms include:
- Frequent, intermittent coughing
- A whistling or wheezing sound when exhaling
- Shortness of breath
- Chest congestion or tightness
- Chest pain, particularly in younger children
- Trouble sleeping caused by shortness of breath, coughing or wheezing
- Bouts of coughing or wheezing that get worse with a respiratory infection, such as cold or flu
- Delayed recovery or bronchitis after a respiratory infection
- Trouble breathing that may limit play or exercise
- Fatigue, which can be caused by poor sleep
How Can Physiotherapist Help?
Physiotherapist role is to provide a clear understanding of asthma, advice and guidance of appropriate exercises to control asthma.
What To Do When Asthma Attacks Happen?
- Begin with effective control breathing
- Take your medication / bronchodilator
- If there is no change within 15 minutes, get emergency treatment at the nearest hospital or clinic
Breathing Control Guide:
- Stop doing the activity.
- Go into relaxation position to facilitate the movement of the diaphragm during breathing
- Do pursed-lip breathing exercises to reduce shortness of breath
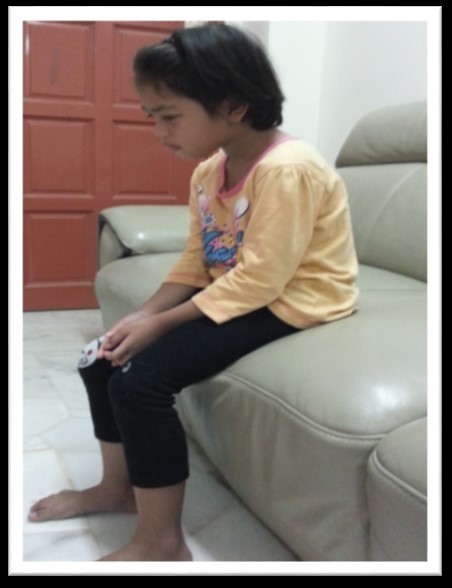
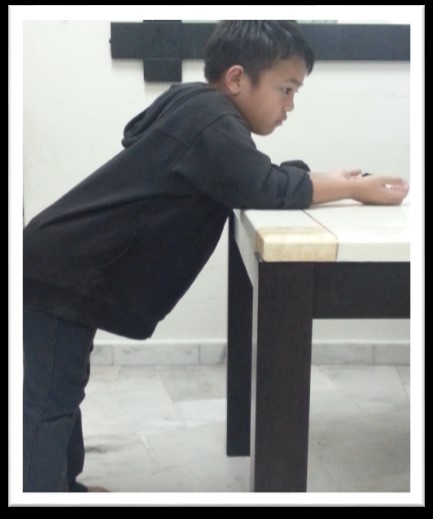
Help Children In Relaxation Position
- Sit with leaning forward / bent forward
- Stand with leaning backward
- Standing with leaning to the side
- Stand with leaning forward
- Lie on your side and lean
Relaxation Guide:
- The position either in standing or sitting
- Bend your head, shoulders and body slightly forward, make sure the shoulders are lifted and rest your hands either on the pillow, table or thigh
- If in sitting, make sure the feet are on the floor
- In standing lean to the side, resting both hands over the side of the body
- In standing lean backward, both feet open slightly
- Make sure the spine is upright.
 |
 |
 |
| Standing leaning to the side | Standing leaning back | Forward bend sitting |
 |
 |
Forward lean sitting
 |
 |
Standing lean forward
 |
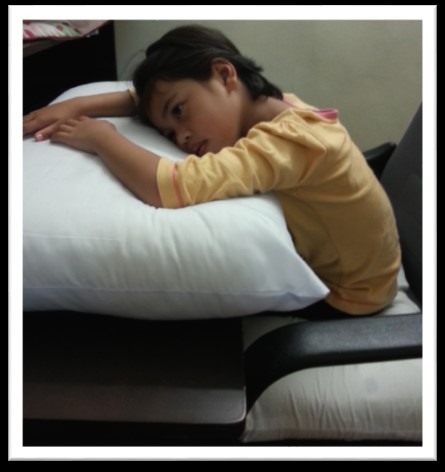 |
| Forward lean sitting on the floor | Forward lean sitting on a chair |
Pursed – Lip Breathing exercise
In any relaxed position:
- Breathe through the nose to the count of 1 or 2
- Breathe out slowly to the count of 1,2,3,4, such as blowing hot air. If it is difficult, blow to the count of 1, 2.
- Do as many as possible to reduce the shortness of breath.

What Should I Do With The Child After Asthma Attack? (Prevention / Rehabilitation)
- Perform proper breathing exercises to enhance the development of the lungs and diaphragm movement
- Encourage effective coughing to facilitate the removal of phlegm
- Do exercises to improve posture
- Take preventive medicines supplied by the doctor.
Diaphragmatic Breathing exercises:
- Sitting, put your hand on your stomach
- Close your mouth and breathe through the nose slowly while bloating stomach and pushing hands up
- Breathe out slowly through the mouth with the deflation of the stomach
- Do at least 3 times in each session
Thoracic Expansion Exercise (TEE):
- Sitting, put your hands on the side of the body
- Breathe through the nose slowly
- Hold the breath for a count of 1,2, 3
- Breathe out through the mouth slowly
- Do at least 3 times per session
Thoracic Mobility Exercise (TME):
- Sitting or standing
- Breathe through the nose while raising both arms slowly up to shoulder level
- Then breathe out through the mouth while lowering both arms slowly to the side of the body
- Do at least 3 times per session
 |
 |
 |
 |
How To Cough Effectively:
- Place your hand on the abdomen
- Take a deep breath through the nose
- Both hands pressing lightly onto the stomach
- Open the mouth and cough
Posture Correction Guide:
- The position either sitting or standing
- Stretch the shoulder and neck, hold the stretch hold for 15 sec.
- Repeat as many as possible at least 5x per session
- Make sure that the body is always upright
 |
 |
 |
What should we do before the child commencing the exercise?
Exercise Guide:
- Make sure the asthma is under control, no shortness of breath and cough
- Take medication before and after exercises
- Wear loose clothing that can easily absorb sweat and sneakers
- Encouraged to exercise in an enclosed area (indoor) when the weather is cold or hazy weather.
- Be sure to accompany children while exercising.
- Start warm-up exercises (warm – up) to avoid injury, such as stretching and breathing exercises for 5-10 minutes
- Then, do activities example long pole, knocking tiger, walking or jogging for 15-20 minutes
- Make sure the exercise is low intensity, so that they are be able to sweat, able to talk and not having difficulty in breathing
- Finish the exercise with stretching and breathing exercises for 5-10 minutes to cool down.
When asthma symptoms occur:STOP THE EXERCISE, TAKE MEDICATION, DO PURSED – LIP BREATHING EXERCISE
References
- Department of Physiotherapy Hospital Sultanah Aminah, Johor Bahru.
- https://www.nlm.nih.gov/medlineplus/ency/imagepages/9248.htm
- https://www.medicalnewstoday.com/info/asthma (What is Asthma? What Causes Asthma?)
- https://www.lung.org/lung-health./lung./asthma (Lung Health and Disease)
- https://www.nhlbi.nih.gov (What To Expect During Pulmonary Rehabilitation)
- http://www.medicinenet.com/asthma_pictures_slideshow/article.htm (Asthma Pictures: inflammatory disorder of the airways)
| Last Reviewed | : | 23 August 2019 |
| Writer | : | Pauzilah binti Hj Dollah |
| Translator | : | Sahira Nadiah Shirlen binti Oyon |
| Accreditor / Reviewer | : | Halimah binti Hashim |







