Ever wonder why your teeth are sensitive, appear short and unsightly? Looks like you might have abnormal tooth wear. So, what is it? You may want to know about it and here, we provide you with the information.
What is tooth wear?
Tooth wear is a multifactorial condition leading to the loss of enamel and dentine. The amount of wear that accelerates physiological tooth wear is referred as pathological or abnormal tooth wear. Abnormal tooth wear can affect the enamel (the first layer of tooth, highly calcified and the hardest tissue in the body), dentine (the second and much softer layer under the enamel) and the nerves and blood vessels (pulp) of the tooth. It is sometimes difficult to determine the type of tooth wear present because different types often occur together. Individuals of all ages can present with the condition.
 |
 |
Complications
Tooth wear may cause problems such as:
- Tooth hypersensitivity
- Pulpal sequelae
- Chewing inefficiency
- Cosmetic problems
Epidemiology
Tooth wear is an increasingly recognised clinical problem. Erosion, a type of tooth wear, is generally considered in Europe to be the most prevalent cause of tooth wear (Bartlett, 2005).
A cross-sectional study involved secondary school children in Kota Bharu area showed that all 16-year-old school children in the sample have some degree of tooth wear with one-fifth of them affected by abnormal tooth wear (Saerah, Ismail, Naing & Ismail, 2006)
Types of tooth wear
There are three types of tooth wear. These are rarely seen in isolation (Ibbetson & Eder, 1999) and often cause patients to seek help from the dentist.
- Abrasion
- Attrition
- Erosion
- What is abrasion?
Abrasion is the loss of enamel and dentine through abnormal mechanical processes involving foreign objects or substances (other than teeth) repeatedly introduced into the mouth and contacting the teeth.
What causes dental abrasion?
- Oral hygiene habits
- Excessive brushing/flossing
- Effect of abrasives in toothpastes
- Personal habits
- Putting foreign objects in the mouth e.g biting pens, placing hair pins, holding pipes with teeth etc)
- Occupational exposure to abrasive particles
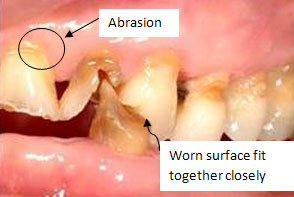
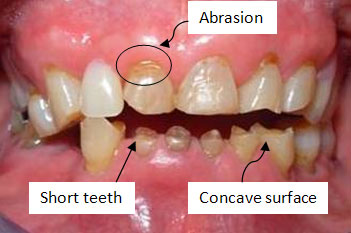
How does dental abrasion look like?
- Usually located at the neck areas of teeth
- Lesions are more wide than deep in dimension
- Premolars and canines are more commonly affected
- Oral hygiene habits
- What is attrition?
Attrition is the loss of enamel and dentine as a result of tooth-to-tooth contact, with no foreign substance intervening.
Grinding (grinding the teeth together) and clenching (squeezing the teeth together) are two of the most common causes of attrition.
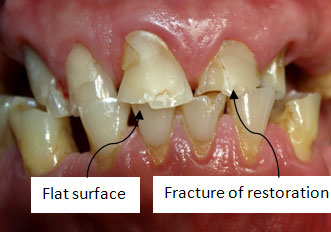
How does dental attrition look like?
- the chewing surfaces become flattened
- enamel and dentine wear at the same rate and the teeth ?t closely together
- shiny facets on amalgam contacts
- possible fracture of cusps of teeth or restorations
- What is erosion?
Erosion is the loss of enamel and dentine due to the presence of acids in the mouth not involving bacteria.
Where is the acid coming from?
- Extrinsic/External acid
- Ingested – e.g acidic food, beverages, medicine. The frequency of acidic foods and drinks and how they are consumed (dietary habits) is important in dietary erosion.
- Working environment – battery sanitary cleanser and soft drinks, manufacturing, plating, galvanizing, acid packing and crystal glassworks etc.
- Intrinsic/Internal acids – acid is from regurgitation of gastric contents, coming in contact with teeth from conditions such as bulimia, anorexia nervosa, chronic alcoholism, morning sickness and gastric reflux.
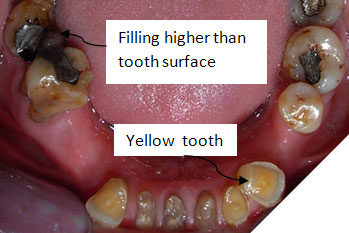
How does dental erosion look like?
- Yellow teeth
- Glazed and smooth teeth
- Loss of surface characteristics of enamel in young children
- Teeth appear to become shorter
- Fillings sit higher than the surrounding tooth surface
- Chewing surfaces of the teeth showsmooth, concave craters
- Sensitive teeth.
- Extrinsic/External acid
Role of acids in erosion
Dietary acids are a common part of modern diets. Generally, a pH value of 5.5 or lower is capable of softening the surface of enamel in only few minutes (Strassler, Drisko & Alexander, 2008). There is strong evidence to suggest that the manner in which the acid food or drink is consumed is more important than the overall quantity.
Examples of acidic foods and drinks commonly associated with erosion:
- soft drinks
- energy drinks
- sports drinks
- alcohol/wine
- fruit juices
- carbonated drink
- pickles
What should I do to minimise the risk of dental erosion? (Lussi & Hellwig, 2006)
- Reduce acid exposure by reducing the frequency and contact time of acids (main meals only)
- Avoid acidic foods and drinks last thing at night
- Avoid sipping, holding or ‘swishing’ acidic drinks around the mouth
- When drinking, use a straw whenever possible as this minimises exposure of the drink to tooth surface
- Do not brush immediately after eating or drinking acidic foods or drinks or after vomitting (erosive challenge)
- Do not brush immediately before an erosive challenge, as the acquired pellicle (thin colourless film on tooth surface) provides protection against erosion
- Use a soft toothbrush and low abrasive fluoride- containing toothpaste
- Chew sugar free gum or lozenges to stimulate saliva flow and wash acids away.
Treatments
Depending on individual cases (abrasion, attrition, erosion or combination), treatment may vary.
- Prevention and monitoring
- Dietary and habit modification
- Splint therapy
- Chemical therapy (e.g fluoride, CCP-ACP, dentine bonding agents)
- Restorations (e.g composite, crowns)
For more information, please consult your dentist in nearby government dental clinic.
References:
- Bartlett D.W. (2005). The role of erosion in tooth wear: aetiology, prevention and management. International Dental Journal. 55. 277-284
- Ibbetson R. & Eder A. (1999). Tooth surface loss: Editor’s introduction. British Dental Journal. 186. 60
- Lussi A, ed. (2006). Dental Erosion: From Diagnosis to Therapy. Basel, Switzerland: Karger; 2006: Whitford GM. Monographs in Oral Science;vol 20.
- Lussi A. (2006). Erosive toothwear: a multifactorial condition of growing concern and increasing knowledge. In: Lussi A, ed. (2006). Dental Erosion: From Diagnosis to Therapy. Basel, Switzerland: Karger; 1-8.
- Lussi A. & Hellwig E.(2006). Risk assessment and preventative measures. In: Lussi A, ed. (2006) Dental Erosion: From Diagnosis to Therapy. Basel, Switzerland: Karger;:190-199.
- Saerah N.B, Ismail N.M., Naing L. & Ismail A.R. (2006). Prevalence of tooth wear among 16-year-old secondary school children in Kota Bharu Kelantan. Archives of Orofacial Sciences. 1. 21-28
- Strassler H.E., Drisko C.L. & Alexander D.C. (2008). Dentin hypersensitivity: its inter-relationship to gingival recession and acid erosion. Inside Dentistry. 29(5 Special Issue):3-4.
| Last reviewed | : | 25 April 2014 |
| Writer | : | Dr. Rosenani bt. Mohd Noordin |
| Accreditor | : | Dr. Chua Meei Jinn |
| Reviewer | : | Dr. Rohani bt. Mahmood |







