The effect of lasers on ocular tissues can be the following:
- Thermal effects
- Photo-disruptive effects
- Photo-ablative effects
An argon laser is a thermal laser. The laser energy is absorbed by the target tissue and is converted to heat and the tissue is coagulated, giving rise to charred rough edges.
A Neodyminium YAG is a disruptive laser. The photodisruptive effect of a YAG laser is to produce a crater like appearance with jagged edges akin to an explosion.


Photoablation is the term used to described absolutely clean, sharp edge without either thermal or mutagenic effects surrounding the wound. This process is achieved by the use of veru high energy to break molecular bonding cleanly, example of photoablation laser is excimer laser.
Laser photocoagulation is use to treat diabetic retinopathy, retinal break, trabeculoplasty, iridoplasty, destructive laser use for laser iridotomy, capsulotomy and photoablation use for refractive surgery.
Pan Retinal Photocoagulation In Diabetic Retinopathy (PRP)
Laser photocoagulation can be used in two scenarios for the treatment of diabetic retinopathy. It can be used to treat macular edema by creating a Modified Grid at the posterior pole and it can be used for panretinal coagulation for controlling neovascularization. It is widely used for early stages of proliferative retinopathy.
Panretinal photocoagulation, or PRP, is used to treat proliferative diabetic retinopathy (PDR). The goal is to create 1,600 – 3,000 burns in the retina with the hope of reducing the retina’s oxygen demand, and hence the possibility of ischemia. It is done in multiple sessions.
In treating advanced diabetic retinopathy, the burns are used to destroy the abnormal blood vessels that form in the retina. This has been shown to reduce the risk of severe vision loss for eyes at risk by 50%.
The laser treatment should be given within 2 weeks after diagnose of PDR, or severe Non Proliferative DR, or diabetic macula oedema. However immediate treatment is recommended for such eye under the following condition:
- Eye with progressive lens changes
- In pregnant patients
- In pre-PDR with diabetic renal failure
- In patients where follow up is doubtful or unreliable
Causes of poor vision in eye with PDR include
- Vitreous haemorrhage (bleeding in the eye)
- Tractional complications with resultant macular detachment displacement and distortion
- Obscurity of macula
 |
 |
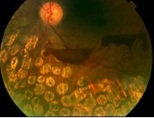
| PDR in Preretinal Haemorrhage | NVD |
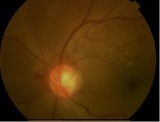 |
 |
| NVD & New Vessels Elsewhere (NVE) | Diffuse Macula Oedema |
Pre-Procedure Preparation
- Doctor will informed regarding the procedure, the treatment helps patient to retain whatever residual vision left in the eye
- Thorough eye examination will be perform before the procedure
- Doctor will ask consent from you
- Your pupil will be dilated before procedure
- Topical anaesthesia will be instilled into your eyes
- Procedure can be done as outpatient
Before using the laser, the eye doctor dilates the pupil and applies anaesthetic drops to numb the eye. In some cases, the doctor also may numb the area behind the eye to reduce discomfort. The patient sits facing the laser machine while the doctor holds a special lens on the eye. The physician can use a single spot laser or a pattern scan laser for two dimensional patterns such as squares, rings and arcs.
During the procedure, you will see flashes of light. These flashes oftentimes create an uncomfortable stinging sensation.
After the laser treatment, you are not advised to drive for a few hours while the pupils are still dilated. Your vision will most likely remain blurry for the rest of the day. Though there should not be much pain in the eye itself, an ice cream headache like pain may last for hours afterwards.
You will lose some of your peripheral vision after this procedure although it may be barely noticeable. The procedure does however save the center of the your sight. Laser surgery may also slightly reduce colour and night vision.
A person with proliferative retinopathy will always be at risk for new bleeding, as well as glaucoma, a complication from the new blood vessels. This means that multiple treatments may be required to protect vision.
Number Of Session Required
Usually 3 sessions are required to complete the treatment of an eye. Patients with logistic problem, should be warded, to capsulate the session within a week duration.
Excessive lader within a short period of time can induce retinal detachment, choroidal effusion and secondary glaucoma.
It is common to have ocular pain while applying laser. This can be overcome by reducing the power. If the pain persists local anaesthesia may be necessary
Follow Up Patient
Laser photopancoagulation is normally repeated 2-3 weeks after the previous session. Once a minimum number of burns have been applied, the eye can reviewed after 4 to 6 weeks. If by this time the new vessels still appear active and there is no sign of regression, one may still add further laser. Sometime further observation is justified as regression may take longer time to be obvious.
Treatment Of Diabetic Macula Oedema
Macula oedema may be focal or diffuse. Macula oedema is related to overall severity and durations of diabetes. It is present in about 10% of all diabetics.
Diffuse diabetic macula oedema is suggested by the presence of diffuse thickening of the macula. Systemic conditions such as hypertension and uremia exacerbate the oedema.
A specific area within the macula will be lasered and it is enough to reduce the oedema or thickening of the macula.
The patient is reviewed 3 to 4 months after the treatment. Repeat treatment is indicated if there is persistence or worsening of macula oedema.
| Last Reviewed | : | 23 August 2019 |
| Writer | : | Dr. Rosniza bt. Ab. Razak |
| Accreditor | : | Dr. Hjh. Nor Fariza bt. Ngah |
| Reviewer | : | Dr. Rosniza bt. Ab. Razak |







