What Is Impacted Tooth?
An impacted tooth is define as failure of a tooth to erupt. When a tooth is impacted, it does not grow into the mouth but stay buried in the jaw bone. Impacted teeth have a major impact on functioning dentition and facial aesthetics of an individual1.
The prevalence of impacted teeth are as follow:
- Central incisors: 0.13%7
- Upper Canine: 1.5%3
- First permanent molar: 0.75% and 6%2,3
Why Do Teeth Become Impacted?
The aetiology for a tooth impaction remains unclear. The possible causes of a tooth failing to erupt include3,5,6:
- Crowding or lack of space for the permanent tooth to erupt
- Presence of an obstruction, such as extra tooth (supernumerary) and fibrous tissue
- Retained deciduous teeth
- Dilaceration of the permanent upper incisor. Dilaceration is resulted from trauma that disrupts root development
- Other pathology such as cysts and odontomes
- Ankylosis, where the root of the tooth become fused to the jaw bone
- Some medical conditions e.g. cleidocranial dysplasia, cleft lip and palate
- Familial history
Treatment Options are:-
Patient and parents counselling on the various treatment options are essential.
- Treatment Principles For Impacted Permanent Upper Incisor3,6,7
Remove retained deciduous tooth - Any retained deciduous tooth should be extracted.
Create and maintain sufficient space - Most of the buried incisors erupt spontaneously when there’s sufficient space.
- Adequate space can be create and/or maintain with fixed or removable braces.
Remove physical obstruction - Any cause of physical obstruction such as an extra tooth (supernumerary), an abnormal mass of tooth structure (odontome), soft tissue thickened (fibrous tissue) and cyst should be removed.
- The buried incisor usually will erupt spontaneously within 16 months after removal of the obstruction.
- Spontaneous improvement is more likely to happen in younger patients.
- If the buried incisor fails to erupt, braces can be used to bring the tooth into the correct position.
- Sometimes, an operation to place a gold chain or brace attachment on the buried incisor is needed to facilitate the tooth movement.
Unfavourable root formation - Sometimes, a buried incisor has abnormal root formation (dilacerated).
- If the dilaceration is mild, the incisor can be aligned with braces.
- Root treatment and/or apicectomy may be required for such teeth.
- If dilaceration is severe, the only option is to remove the incisor completely by surgery.
Incisor removal and space management - If a permanent incisor has been removed, there will be a gap.
- This gap can be closed with braces. Then, the adjacent teeth are reshaped to mimic the missing incisor.
- The gap can be also restored with denture, bridge, implants or an autotransplantation tooth.
- Autotransplantation involves placement of the patient’s own developing premolar to replace the missing incisor. This premolar will need some reshaping to mimic the incisor.
Ankylosed maxillary incisors - Sometimes, the incisor is fused to the bone and will not move (ankylosed).
- The ankylosed incisor can be extracted. The gap then can be restored with denture, bridge or implants.


Insufficient space for the eruption of an impacted upper right incisor
Eruption of an impacted upper left incisor obstructed by a supernumerary
- Treatment Options For Impacted Permanent Maxillary Canine1,2,3,4,5
Option 1: No Treatment and Observe - No treatment.
- Leave the buried canine where it is if it is not causing any problems.
- Indicated for patient who is not keen to undergo treatment.
- The buried canine may be x-rayed occasionally to check the tooth is not causing problems.
- There is a potential risk that the buried tooth could damage the roots of the adjacent teeth or a cyst may form around the buried canine.
- If the primary canine is still present, it can be kept, but it may not last a lifetime.
- If the primary tooth is lost during adulthood, there will a gap. The gap may be restored with denture, bridge or implant.
Option 2: Extraction of the Retained Primary Canine - Timely extraction of the primary canine in patients aged 10-13 years old, may help to normalize the eruptive path of the canines.
- If there is no sign of radiographic improvement after 12 months, it is unlikely to occur and other options should be considered.
Option 3: Surgical Exposure and Orthodontic Alignment - Indicated for well-motivated patients where the canine is in a favourable position.
- Surgical exposure is an operation where a small ‘window’ of gum and bone is removed around the buried tooth to help it grow into the mouth.
- This operation will involve either a general or local anaesthetic.
- Sometimes, a gold chain or brace attachment is placed on the tooth during the time of operation.
- Fixed braces are used to bring the canine tooth into the correct position.
- Moving an impacted canine can be a very slow process. It can often take more than 2 years for the treatment to be completed.
- Very rarely, the buried canine ankylosed. If this happens, the only option may be surgically remove the tooth.
Option 4: Surgical Removal - This is an operation to remove the buried canine completely.
- Indicated when the canine is in a poor position.
- It is suitable in patient who does not want to wear fixed braces.
Option 5: Autotransplantation - This is an operation involves the surgical removal of the buried canine and subsequently ‘transplant’ it into its proper position.
- It may be considered when the canine has a poor position and there is enough space between the teeth to accommodate the canine.
- A short period of orthodontic treatment may be needed to create sufficient space for the implantation of the canine.
- This option is not often chosen and can only be considered in certain cases as it has a lower success rate than the other options.
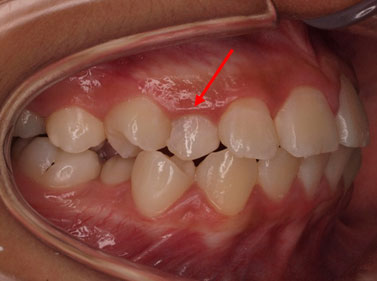

Impacted upper right canine with retained primary canine
Timely extraction of the primary canine may help to normalize the eruptive path of the impacted canine

 Fixed braces and a gold chain are used to bring the impacted canine into the correct position
Fixed braces and a gold chain are used to bring the impacted canine into the correct position - Treatment Principles For Impacted Permanent Premolar In cases where a premolar is unerupted, consideration can be given to extract the first premolar which has erupted. Orthodontic braces can be used to maintain the extraction space while waiting for the spontaneous eruption of the impacted premolar3.
- Treatment Principles For Impacted Upper First Permanent Molar2,3
Observation - In mild cases, the impacted molar should be observe for a period of time.
- A large portion of these molars will self-correct.
- If there is no spontaneous improvement within 3-6 months, active treatment should be undertaken.
Separation - A brass wire or an elastic separator can be used in an attempt to separate the permanent molar from the second primary molar.
Orthodontic treatment - Orthodontic appliances such as removable appliances, fixed appliances or headgear can be used to disimpact the first permanent molar.
Extraction of the second deciduous molar - Extraction of the second primary molar is the final option.
- This option is considered when the primary molar has severe root damage.
- This option is likely to lead to space loss and future crowding in the second premolar region.
Conclusion
Management of patient who present with impacted teeth is different. This is a general information on the possible treatment options available. For further help and advice, talk to your orthodontist or dentist.
References
- British Orthodontic Society (2015). Patient information leaflets: Impacted canines. Retrieved March 31, 2015 from http://www.bos.org.uk/Portals/0/Public/docs/PILs/impactedcaninesnovember2013.pdf
- Cobourne, M.T., & DiBiase A.T. (2010). Handbook of Orthodontics. Philadelphia: Mosby Elsevier.
- Gill, D.S. (2008). Orthodontics at a Glance. West Sussex: Blackwell Munksgaard.
- Husain, J., Burden, D., McSherry, P., Morris, D., & Allen, M. (2012). National clinical guidelines for management of the palatally ectopic maxillary canine. British Dental Journal, 213, 171-176.
- Ministry of Health Malaysia. 2004. Clinical Practice Guidelines: Management of the palatally ectopic canine.
- Ministry of Health Malaysia. 2006. Clinical Practice Guidelines: Management of unerupted maxillary incisor.
- Yaqoob, O., O’Neill, J., Gregg, T., Noar, J., Cobourne, M., & Morris, D. (2010). Management of unerupted maxillary incisors. The Royal College of Surgeons of England.
- Ortho Technology. (2015). Image of Gold Chain. Retrieved April 05, 2015 from http://www.orthotechnology.com/new_products/eruptionappliance.cfm
| Last Reviewed | : | 16 February 2016 |
| Writer | : | Dr. Then Poh Kiun |
| Accreditor | : | Dr. Rafeaah bt. Ayat Khan |
| Reviewer | : | Dr. Hjh. Rashidah bt. Dato’ Hj. Burhanudin |







