What is meningitis?
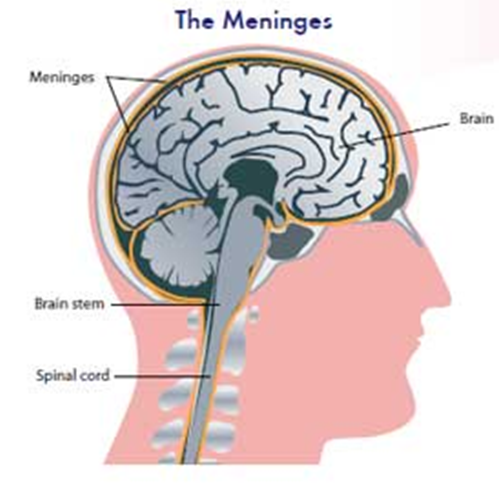
- Meningitis is an inflammation of the meninges, the lining of the brain. It is almost always caused by germs (bacteria, viruses, tuberculous and others). The bacteria that most often cause meningitis in children are of the species Haemophilus influenzae, Streptococcus pneumoniae and Neisseria meningitides. More than 90% of the cases involve children under 5 years old and 50% were among infants under 6 months old.
 |
How Can A Child Get Meningitis?
- Meningitis usually results from bloodstream infection after a child contracted the offending germs. These germs or bacteria usually enter the body through the respiratory tract. Fortunately not many people who get respiratory tract infection will go on to develop blood stream infection. Those who develop blood stream infection will not necessarily develop meningitis because the brain is protected by blood-brain barrier, unless this barrier is weakened due to the infection itself or other causes.
- Sometimes meningitis can develop due to direct spread of severe infection from the ear (otitis media) or nasal cavity (sinusitis).
- Injury or surgical procedure around the skull and face also may increase the risk of meningitis.
What are the signs and symptoms?
Signs and symptoms of meningitis in children are dependent on the patient’s age, types of bacteria, whether antibiotic has been started and the duration of illness. Early symptoms:
- High fever.
- Irritability.
- Lethargy.
- Poor feeding or food refusal.
- Headache and vomiting.
- Skin rashes that spread rapidly to the whole body (if due to the bacteria Neisseria meningitides).
Late symptoms:
- Bulging fontanelle (soft spot on a baby’s head).
- Stiff neck.
- Seizures.
- Very drowsy and difficulty in waking up.
- Coma.
How is meningitis diagnosed?
The diagnosis of meningitis can only be confirmed through examination of a small sample of spinal fluid through a procedure called lumbar puncture (see the topic ‘Lumbar Puncture’). This procedure is also important to determine the type of infective germ so that the patient could be treated with the appropriate antibiotics.
What are the complications of meningitis?
Meningitis is a serious disease. It may cause death in 10% of patients and 30% of the survivors have serious long term complications. Early treatment with appropriate antibiotics given at adequate duration is essential to prevent or reduce these complications. Long-term complications that may occur include:
- Pus collection within the brain or the skull (subdural effusion/brain abscess).
- Hydrocephalus (Obstruction to the flow of cerebrospinal fluid leading to rapidly enlarging head).
- In the above 2 conditions, the patient may need to undergo surgical procedures for further treatment.
- Learning disability.
- Hearing loss/speech and language impairment.
- Visual impairment.
- Paralysis/Cerebral palsy.
What is the treatment of Meningitis?
- Appropriate antibiotics are usually given for one to two weeks depending on the type of infective bacteria and the patient’s response to the treatment given.
- Unconscious patients or those with recurrent seizures are often nursed in intensive care unit. They may need to be put on a ventilator to assist in breathing. Specific treatments may also be required to control seizures, reduce brain swelling and pressure inside the skull.
How can meningitis be prevented?
- Some forms of bacterial meningitis can be prevented through childhood immunizations. Consult your doctor.
- To prevent meningitis from spreading among family members or close contacts especially to other children aged less than five years old, certain antibiotic will be given to the high risk group if the patient was infected by the bacteria Haemophilus influenzae or Neisseria meningitides.
| Last Reviewed | : | 27 April 2012 |
| Content Writer | : | Dr. Khoo Teik Beng |
| Reviewer | : | Dr. Nor Azni b. Yahaya |







