Timed ntercourse
It is the act of having sexual intercourse on the most fertile days of a woman’s monthly cycle. This is a treatment option for infertility. It is often used by young couples with unexplained infertility, who want a simple and natural choice to conceive.
Ovulation is stimulated with oral medication that improves the selection and maturation of eggs (Clomiphene Citrate). Follicular growth is then monitored via trans-vaginal ultrasound. Ovulation is induced with a subcutaneous HCG injection when scan shows the egg is mature. Couples will be asked to have sexual intercourse 24 to 48 hours after administering the HCG.
Most pregnancies achieved via this treatment happen in the first 3 or 4 months. If the couple fails to conceive beyond this time, other options should be considered.
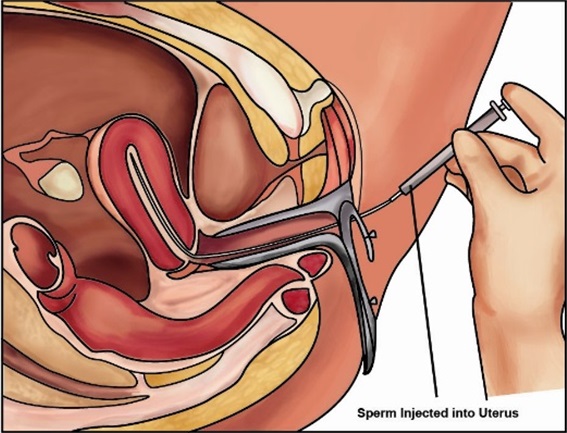
What is IUI?
Intrauterine insemination (IUI) involves placing the fast moving sperm of the husband into the wife’s womb close to the time of ovulation or when the egg is released from the ovary. It involves a laboratory procedure to separate fast moving sperm from the more sluggish or non-moving sperm. IUI can be done with or without fertility drugs which boost egg production. The fallopian tubes must be normal and not blocked for this mode of infertility treatment to be considered.
How does IUI work?
The husband is asked to produce a sperm sample on the day the intrauterine sperm insemination takes place. Sperm are washed to remove the fluid surrounding them and the rapidly moving sperm separated out. The rapidly moving sperm are placed in a small catheter (tube) which will be inserted into the womb.
If fertility drugs are not used, IUI is done between day 12 and day 16 of the menstrual cycle – with day one being the first day of period. A urine ovulation predictor kit can be used to detect the hormone surge that signals imminent ovulation.
If fertility drugs are used to stimulate ovulation, vaginal ultrasound scans are used to track the development of the eggs. As soon as an egg is mature, the patient is given a hormone injection to stimulate its release. The sperm is inseminated 36 to 40 hours later. The doctor first inserts a speculum (a special instrument that keeps your vaginal walls apart) into your vagina (as for a cervical smear test).
A small catheter (a soft, flexible tube) is then threaded into the womb via the cervix. The washed sperm is then inseminated into the womb through the catheter. The whole process takes just a few minutes and is usually a painless procedure but some women may experience a temporary, menstrual-like cramping. The patient can rest for a short time before going home.
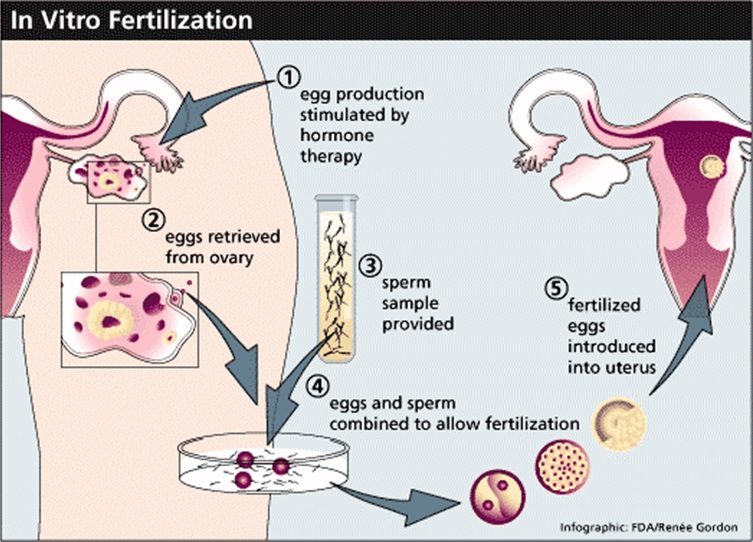
IVF- What is IVF?
In vitro fertilisation (IVF) (which actually means ‘fertilisation in glass’) is synonymous with the term ‘test tube baby’. During the IVF process, eggs are removed from the ovaries and fertilised with sperm in the laboratory. The fertilised egg (embryo) is later placed in the woman’s womb.
IVF may be recommended if the patients:
- have been diagnosed with unexplained infertility
- fallopian tubes are blocked
- have been unsuccessful with other techniques like using fertility drugs or intrauterine insemination (IUI)
- there is a minor degree of male subfertility – more severe problems are treated with intra-cytoplasmic sperm injection (ICSI).
In the IVF process, the woman will receive a drug to suppress her natural cycle. Treatment is given either as a daily injection (which is normally self-administered unless the patients are not able to do this herself). This continues for about two weeks.
Then after the natural cycle is suppressed, she is then given a fertility hormone called FSH (or Follicle Stimulating Hormone). This is usually taken as a daily injection for around 10-12 days.This hormone will increase the number of eggs she produces – meaning that more eggs can be fertilised. With more fertilised eggs, the IVF has a greater choice of embryos to use in her treatment.
Throughout the drug treatment, the doctor will monitor the patient’s progress. This is done by vaginal ultrasound scans and, possibly, blood tests. 34–38 hours before her eggs are due to be collected, a hormone injection to help her eggs mature.
In the IVF process eggs are usually collected by ultrasound guidance under sedation through the vagina. This involves inserting a needle which is attched to a trans-vaginal ultrasound probe and the needle is then inserted into each ovary to obtain eggs. Cramping and a small amount of vaginal bleeding can occur after the procedure.
Around the time the patient’s eggs are collected, the husband is asked to produce a fresh sample of sperm. This is stored for a short time before the sperm are washed and spun at a high speed. This is so the most active sperm can be selected.
The woman’s eggs are mixed with her husband’s sperm in a special dish and cultured in the laboratory for 16–20 hours. They are then checked to see if any have been fertilised. Those that have been fertilised (now called embryos) are grown in the laboratory incubator for another one – two days before being checked again. The best one or two embryos will then be chosen for transfer. After egg collection, the patient are given medication to help prepare the lining of the womb for embryo transfer. This is given as pessaries, injection or gel.
For women under the age of 40, one or two embryos can be transferred. If you are 40, or over, three embryos can be used. The number of embryos being transferred is restricted because of the risks associated with multiple pregnancies. Remaining embryos may be frozen for future IVF attempts, if they are suitable.
Some clinics may also offer blastocyst transfer, where the fertilised eggs are left to mature for five to six days and then transferred. (see Embryo transfer and Blastocyst transfer)
What is intra-cytoplasmic sperm injection (ICSI) and how does it work?
Intra-cytoplasmic sperm injection (ICSI) involves injecting a single sperm directly into an egg in order to fertilise it. The fertilised egg (embryo) is then transferred to the woman’s womb. The major development of ICSI means that as long as some sperm can be obtained (even in very low numbers), fertilisation is possible.
ICSI is often recommended if:
- the husband has a very low sperm count
- other problems with the sperm have been identified, such as poor morphology (abnormally shaped) and/or poor motility (poor swimmers)
- at previous attempts at in vitro fertilisation (IVF) there was either failure of fertilisation or an unexpectedly low fertilisation rate
- the male partner has had a vasectomy and sperm have been collected from the testicles or epididymis (sperm reservoir)
- other situations where the sperm count is zero and donor insemination is not wanted
- the husband does not ejaculate any sperm but sperm have been collected from the testicles
- the husband has had problems obtaining an erection and ejaculating. This includes men with spinal cord injuries, diabetes and other disorders.
The procedure for ICSI is similar to that for IVF, but instead of fertilisation taking place in a dish, the embryologist selects sperm from the sample and a single sperm is injected directly into each egg. This does not mean that the egg is fertilised, but ICSI now gives an opportunity for that complex process to commence. ICSI is not a guarantee that fertilisation will take place.
An embryologist will examine the sperm under a microscope and decide whether ICSI could increase the chances of fathering a baby. The next step depends on whether the husbands are able to provide sperm without medical intervention. Subsequently one – three of the best quality embryos are transferred to the womb.
In case of zero sperm count (Azoospermia)
If the husbands have a zero sperm count (other than caused by vasectomy), the chances of retrieving sperm surgically by PESA, TESA or TESE may be very low or at least uncertain. In this situation, consider having a surgical retrieval such as a ‘dummy run’ and store any sperm that are obtained. Sperm can be collected directly from the epididymis (a narrow tube inside the scrotum, where sperm are stored and matured) using a type of fine syringe. This is known as ‘percutaneous epididymal sperm aspiration’ or PESA.
Sperm can also be retrieved from the testicles, a process known as ‘testicular sperm aspiration’ or TESA.
It is also possible to remove tiny quantities of testicular tissue from which sperm can be extracted. This procedure is called ‘testicular sperm extraction’ or TESE.
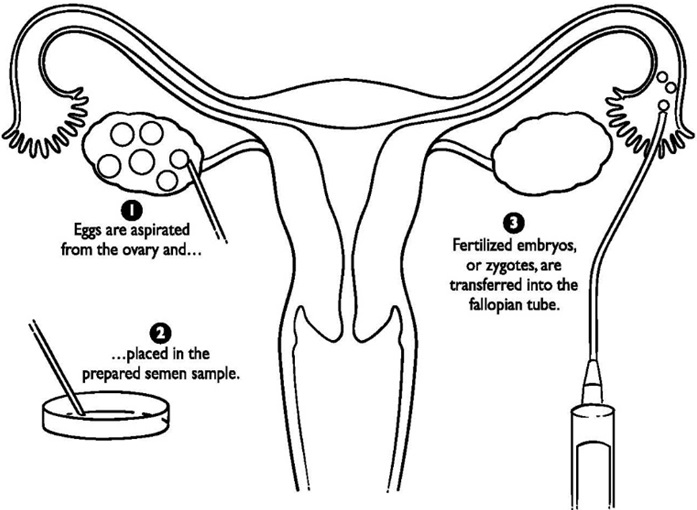
What is GIFT?
With gamete intra-fallopian transfer (GIFT), the preparation and monitoring of the growth of eggs is identical to in vitro fertilisation (IVF).
Instead of the eggs being fertilised “in vitro” in the laboratory, the healthiest eggs and sperm are placed together in the woman’s fallopian tubes. Fertilisation therefore takes place in the body, as it would if conception had occurred naturally.
GIFT has been used with some success in cases where:
- a couple has unexplained infertility
- the woman’s fallopian tubes aren’t blocked or damaged
- the man has a low sperm count, or there are problems with the sperm
- there are objections to IVF on religious or other reasons
- IVF has failed to result in a successful pregnancy.
However, the clinical guidelines on fertility issued by NICE (the National Institute for Health Clinical Excellence) state:
‘There is insufficient evidence to recommend the use of gamete intrafallopian transfer … in preference to in vitro fertilisation in couples with unexplained fertility problems or male factor fertility problems.’
Before proceeding with GIFT, it is essential that the fallopian tubes are known to be open and healthy. A tubal patency test is usually carried out as part of the assessment by the doctor. Up to the point of egg collection, the procedure for GIFT is the same as that for IVF (see IVF). The patient will be anaesthetised and the doctor will make a small 5mm cut at the umbilicus. This is so they can insert a laparoscope to view the womb and fallopian tubes.
On the same day that the eggs are collected, the husband is asked to provide a sperm sample and are being mixed with eggs in the catheter and deposited in the fallopian tubes.
Under direct vision through the laparoscope, eggs are removed from the ovaries. This may require two additional small incisions in the lower abdomen. Up to three of the best quality eggs (if below the age of 40, or up to four eggs if over 40) are then mixed with the prepared sperm in a catheter (a fine, flexible tube). The doctor inserts the catheter via the laparoscope into the end of one or both fallopian tubes and deposits the eggs and sperm. The patient need a short rest before going home and she will be given medication to build up the lining of her womb and provide a good environment for any fertilised eggs.
Currently, there are no clinic in Malaysia that offer GIFT.
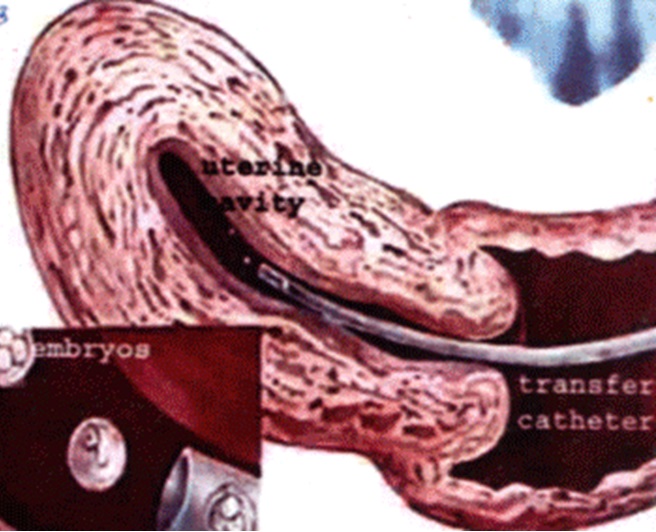
What is embryo transfer?
Embryo transfer takes place after eggs have been collected and fertilised in the laboratory. Depending on the situation between one and three of the best quality embryos are selected and then transferred to the woman’s womb. An embryo must successfully attach itself to the wall of the womb for pregnancy to begin.
A typical procedure may involve the following:
Two to three days after the eggs are fertilised, the best quality embryos are selected to be transferred to the womb. If the patients are under the age of 40, one or two embryos can be replaced, but if 40 or over, three embryos can be used.
If the women have good quality embryos, those that are not transferred can be frozen. Some clinics may also offer blastocyst transfer, where embryos are transferred five to six days after fertilisation.
The doctor doing the embryo transfer inserts a speculum into the vagina. This is the same procedure as a cervical smear test where the speculum is used to keep her vagina’s wall apart. A fine tube (catheter) is passed through the cervix, normally using ultrasound guidance. The embryos are passed down the tube into the womb.
This is normally a pain-free procedure and usually no sedation is necessary, but the patient may experience a little discomfort because a full bladder is needed if ultrasound is used.
It is generally recommended that the patient lead a gentle lifestyle during the few days after embryo transfer. Hospital admission is not necessary. About two weeks after the embryo transfer, a pregnancy blood test is done. If it is positive then a scan about two weeks later is performed.
There are no significant risks relating to the embryo transfer process itself.
Reference
- http://www.hfea.gov.uk/IUI.html
| Last Reviewed | : | 23 February 2019 |
| Writer | : | Dr. Hj. Mohamed Hatta b. Mohamed Tarmizi |
| Accreditor | : | Dr. Haris Njoo Suharjono |
| Reviewer | : | Dr. Rafaie bin Amin |