Meeting the nutritional requirements of preterm baby represents a continuing challenge facing doctors, nurses, as well as the baby’s family. Nutrition during early life is now recognized not only as a key determinant for immediate neonatal survival, growth and mental development during infancy, but also as a major conditioning factor for long-term health. Preterm babies very often need admission to neonatal intensive care unit after birth. This make breastfeeding a little more challenging. However, most mothers are able to express their breast milk to feed their little ones.
Expressed breast milk (EBM)
Breast milk is the feed of choice for preterm baby. Besides providing nutrients needed for growth and development, human milk also contains numerous immune-protective components that protect the premature babies from infection. However, most of the preterm babies are unable to feed directly from mother’s breast at the initial stage due to their sickness or immaturity of sucking-swallowing reflex. Therefore it is very important for a mother to express her breast milk so that her baby can still receive breast milk using alternative methods such as orogastric tube feeding, cup feeding etc.
EBM expression and storage
Clean your hands before expressing breast milk. Express breast milk in a clean container. Write the date and time on the EBM container each time after expressing. Do not mix EBM at different time in a same container. You can consult local healthcare staff in wards/ clinics regarding technique of expressing, storing and transporting EBM.
After expressing, EBM should be kept in the fridge/ freezer if not sending to hospital immediately. You can store your EBM in a number of ways as follow:
|
Place |
Temperature |
Duration |
| Fridge |
? 4°C |
24 hours |
| Freezer compartment inside refrigerator |
-15°C |
2 weeks |
| Freezer section of refrigerator with separate door |
-18°C |
3 months |
| Freezer |
? -18°C |
6 months |

Storing EBM in the fridge
How to transport expressed breast milk to hospital
When transporting EBM to hospital, keep the EBM in a cold environment such as by using a cooler.

Example of a cooler
Human milk fortification (HMF)
Preterm babies often need HMF to be added in EBM. The aim of fortification is to raise the concentrations of specific nutrients in relation to energy to such levels that nutrients needs are met whenever energy needs are met.
Total parenteral nutrition (TPN)
Preterm babies are born with limited nutrient stores, and take time to establish enteral feeding. Most babies < 32 weeks or < 1500g will require TPN at the initial stage while establishing enteral feeding. TPN is a type of nutritional formula giving intravenously to the baby. It contains nutrients such as glucose, protein, fat, vitamin and dietary minerals. TPN is an important source of energy and nutrients when the baby is still not on full enteral feed.

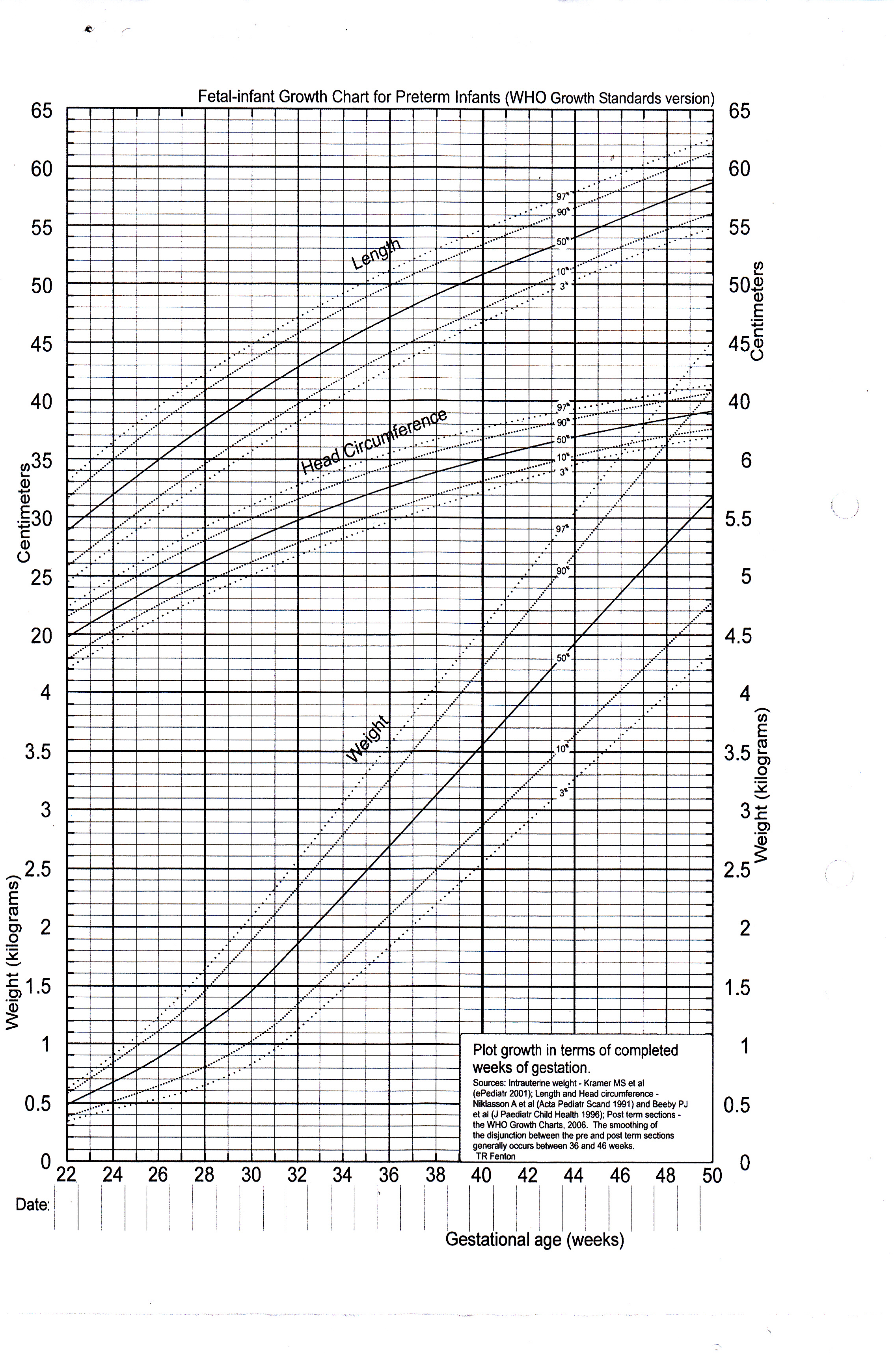
Growth monitoring
Preterm growth is usually monitored by checking the weight, head circumference and length regularly. The growth parameters will then be plotted on a growth chart to monitor the trend of the growth. Higher growth velocity on the neonatal intensive care unit that was similar to intrauterine growth rates predicts better neurological outcome.
Growth Chart
Feeding the preterm babies after discharge
The very preterm infant at the time of discharge represents a nutritional challenge to healthcare providers as well as infant’s family on the decision on what type of milk should be given after discharge and on the need to continue to supplement mother’s milk. The World Health Organization, American Pediatric Society, and European Society for Paediatric Gastroenterogy Hepatology and Nutrition (ESPGHAN) recommend mothers’ own milk for nutrition of infants for the first 6 months of life and beyond. Close monitoring of feeding and growth is recommended after hospital discharge.
References:
- B. Koletzko et al. Nutritional Care of Preterm Infants.2014;110.
- C. Agostoni et al. Enteral Nutrient Supply for Preterm Infants: Commentary From the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition Committee on Nutrition. JPGN. 2010;50(1).
| Last Reviewed | : | 28 Oktober 2015 |
| Writer | : | Dr. Leong jen Jen |
| Accreditor | : | Dr. Neoh Siew Hong |