Periodontitis is a series of chronic gum inflammation involving the destruction of the structures supporting the teeth, i.e. gingiva, periodontal ligament, cementum and alveolar bone. (Diagram 1)
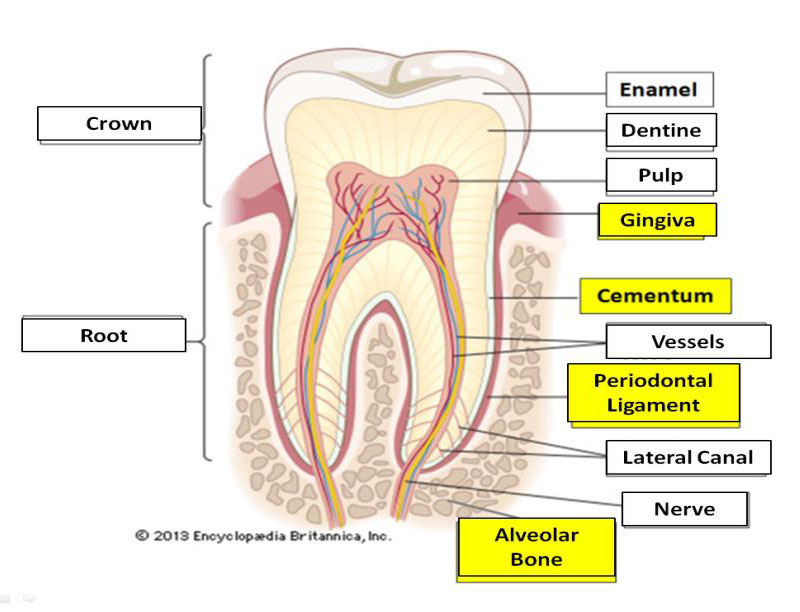
Diagram 1: The Periodontal Tissues
Gum inflammation is caused by the accumulation of microorganisms present in the dental plaque.
In the initial stage of the disease or Gingivitis, inflammation is only limited to the gum. The signs observed are gum redness and swelling, bleeding on tooth brushing, changes in gum shape and pus discharge. Patients may also complain of bad breath.
Gingivitis can heal well after a few visits to the dentist and given treatment such as scaling, prophylaxis and oral hygiene instructions.
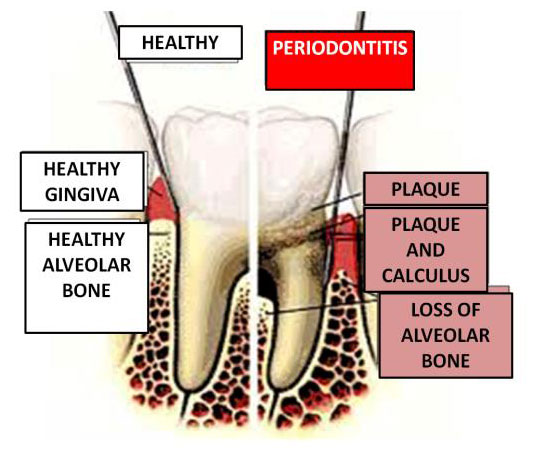
On the other hand, if gingivitis is neglected without any treatment done, the inflammation may spread to other periodontal structures leading to permanent alveolar bone loss, known as Periodontitis.
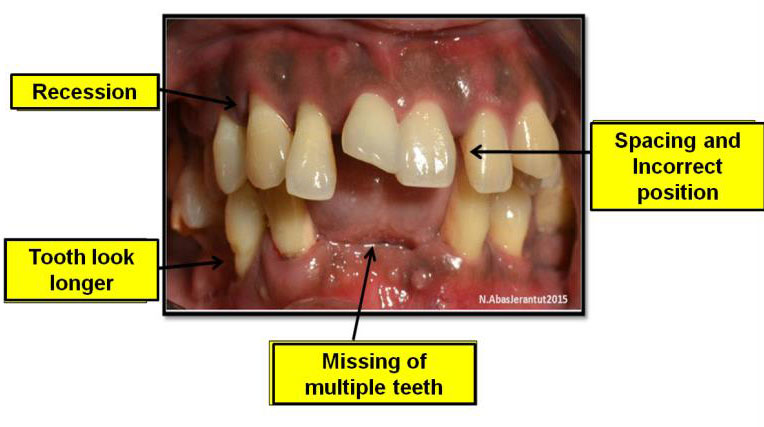
The progressive loss of the tooth-supporting structures such as alveolar bone and periodontal ligament (Diagram 2) will result in :
- Gum recession
- Teeth appears to be elongated
- Mobile teeth
- Drifting of teeth with apparent spacing or crowding (Diagram 3).
- Difficulty in chewing, especially hard or sticky food.
- Foul mouth odour
Unfortunately, most patients are unaware of this condition since they do not experience pain due to periodontitis, until they have a periodontal examination done at a dental clinic or inform the dentist about the symptoms.
 |
 |
|
Diagram 2: Periodontitis |
Diagram 3: Signs of periodontitis |
Clinically, the dentist will carry out a basic periodontal examination, using the periodontal probe (Diagram 4) to measure the depth of a periodontal pocket. If the periodontal pocket is more than 4mm deep, it is likely to assume that periodontitis has occurred.
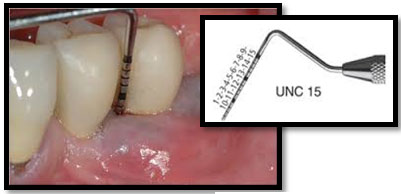
Diagram 4: Measuring the periodontal Pocket
Risk factors associated with periodontitis.
Local factors include conditions which encourage plaque retention , such as teeth crowding, presence of dental caries, uneven fillings surfaces and overhanging fillings.
Systemic factors are those that contribute effects to the body, example genetic factors, systemic diseases and smoking habit.
Several studies have established an association between periodontitis and systemic diseases such as diabetes mellitus, heart disease, low birth weight, premature birth and obesity.(1,2)
Obesity and overweight is defined as “abnormal or excessive fat accumulation that presents a risk to health” (WHO 2008).
In developed countries, there is an increase in the prevalence of overweight and obesity in the population. Obesity has been identified as the main cause for chronic diseases like heart disease, diabetes mellitus, cancer and osteoarthritis.
There are several ways to measure obesity; the most commonly used is the Body Mass Index (BMI).
BMI calculation:
weight (kg)
height (m)2
The following is the BMI chart according to WHO 2008 :
|
Class |
BMI (kg/m2) |
Description of population |
|
Underweight |
<18.5 |
|
|
Normal |
18.5-24.9 |
Normal |
|
Overweight |
?25.0 |
Increased |
|
Pre-obese |
25-29.9 |
|
|
Obesity class 1 |
30.0-34.9 |
High |
|
Obesity class 2 |
35.0-39.9 |
Very High |
|
Obesity class 3 |
?40 |
Extremely High, health risk |
Obesity associated with periodontal disease?
Studies have shown a positive correlation between obesity and the occurrence of periodontitis(4) with a statistically significant association between periodontitis and obesity (odd ratio: 1.81) and overweight (odd ratio: 1.27) (5).
Nevertheless, more additional prospective studies are required to quantify the mechanisms of this association and provide sufficient evidence for guidelines on the clinical management of periodontitis in obese patients.
How does obesity cause periodontitis?
Among the contributory factors related to the occurrence of periodontitis among obese patients are:
- The increase in the level of immune cells and inflammatory mediators, i.e. acute phase protein, leucocytes and pro-inflammatory cytokines.
- Adipocytes cell in obese patients produce more inflammatory factors such as IL-1, IL-6, TNF-? and chemokines which can lead to red and swollen gums, loss of alveolar bone and periodontal ligament in periodontitis.
- The amount of bacteria inside the oral cavity of an obese individual is found to be higher than those with normal body weight.
- There is also an association between obesity and diabetes mellitus whereby the insulin hormones become less sensitive and form high amount of advance glycation end product (AGE) leading to more inflammation of the periodontal tissues.
Periodontitis has multi-factorial causes which include genetic factor, smoking habit, imbalance diet and unhealthy lifestyle (Diagram 5).
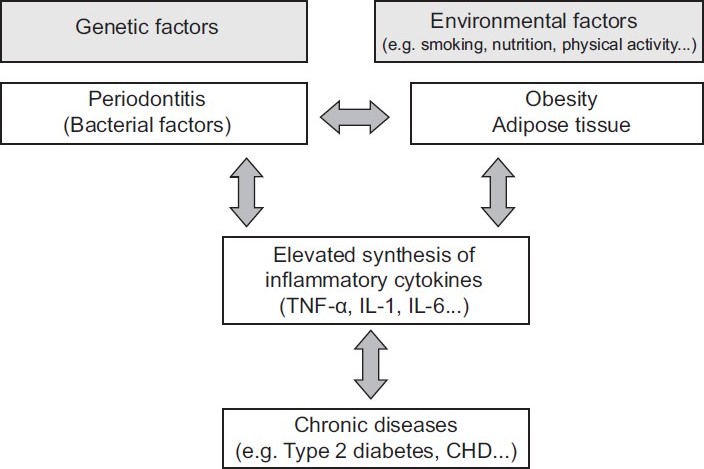
Diagram 5: Possible Mechanism Of Association Between Obesity And Periodontal Disease
How is Periodontal disease managed?
Patients who exhibit the signs and symptoms of gum disease are advised to visit a dentist for further examination. The dentist would advise on the proper care of the teeth and gums.
If periodontitis has established, patient will be referred to a Periodontal Specialist for further periodontal treatment which include:
- Scaling, to remove the plaque and calculus.
- Root surface debridement for gums with deep pockets (6mm and above)
- Severe cases may require periodontal surgery for correction of defects or uneven root and bone surfaces caused by the bacterial infection.
These are some of the ways to prevent periodontitis and obesity:
- Maintaining excellent oral hygiene by brushing your teeth with the correct technique, at least twice a day with fluoridated toothpaste to prevent caries. You are also encouraged to use dental floss to remove food debris and plaque interdentally.
- Healthy diet. Reduce sugar intake and oily food for your oral and overall health. Increase intake of high-fiber vegetables and fruits. You are also encouraged to consume high calcium food and drink for stronger bones and teeth.
- Dental checkup at least once a year helps in detecting and treating the disease at an early stage.
- Exercise frequently and aim for an ideal body weight.
References
- Saito T, Shimazaki Y, Koga T, Tsuzuki M, Ohshima A.Relationship between upper body obesity and periodontitis. J Dent Res 2001:80:1631-1636.
- Saito T, Shimazaki Y, Sakamoto M. Obesity and periodontitis. N Engl J Med 1998; 339:482-483.
- WHO. Global database on body mass index. 2008. Report.
- Dalla Vecchia, C.F., Susin, C., Rösing, C.K., Oppermann, R.V. and Albandar, J.M., 2005. Overweight and obesity as risk indicators for periodontitis in adults. Journal of Periodontology, 76(10), pp.1721-1728.
- Suvan, J., D’Aiuto, F., Moles, D.R., Petrie, A. and Donos, N., 2011. Association between overweight/obesity and periodontitis in adults. A systematic review. Obesity Reviews, 12(5), pp.e381-e404.
| Last Reviewed | : | 19 June 2017 |
| Writer / Translator | : | Dr. Norhayati bt. Abas |
| Accreditor | : | Dr. Norhani bt. Abd Rani |







