Source: images.search.yahoo.com
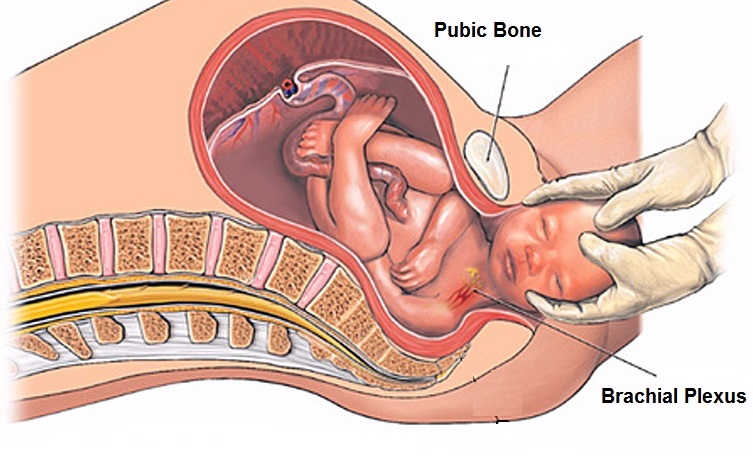
Obstetric Brachial Plexus Palsy (OBPP) is defined as brachial plexus nerve injury that occurs during early delivery. Incident of OBBP is totally different with the adult brachial plexus injury. Eg fall on outstretch hand is one of the cause among the adults. In contrast, occurrence of the OBPP among neonate/ infant during delivery would cause incomplete rupture because of abnormal muscle stretch around the neck.
Etiology
OBBP commonly happen during delivery process and resulting in overstretch of the neck. The incident ratio among neonate is 1 and 2: 1000 delivery. Almost 90% of them would recover completely in a year of their life and the remaining 10% will need therapy. Surgery would be done on the severe cases. Hence, most of them might have limitation of their body function for the entire life.
Brachial Plexus Injury can be divided into 3 difference types depending on the nerve level:
- Erb’s Palsy which involved the upper brachial plexus (C5, C6 & C7): Only can move the fingers. Shoulder will be completely paralyzed
- Global/Total Obstetric Brachial Plexus Palsy (OBBP) which involves both upper and lower brachial plexus (C5-T1): More severe compare to Erb’s Palsy.
- Klumpke’s Palsy involves forearm and hand . (C8 & T1):
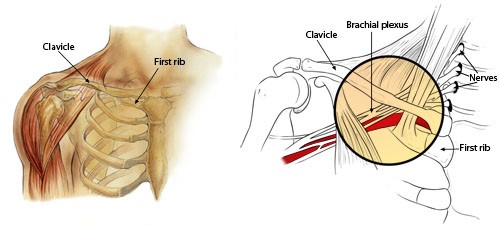
Anatomy
Source: images.search.yahoo.com
Brachial plexus nerves innervates upper trunk, arms, forearms and the hands. Its consists of cervical nerves (C5 – T1) and merged to become the nerve plexus. Its divide into 3 parts , upper trunk (C5-C6), middle trunk (C7) and lower trunk (C8 dan T1).
Types of Nerve Injuries
- Neuropraxia
- Neuroma
- Rupture
- Avulsion
Causes
- Cephalopelvic disproportion
- A large or macrosomic baby
- Instrumental delivery eg forcep
- Delivery
- Premature delivery
- Shoulder dystocia
- Primigravida
- Prolong delivery
- Injury when delivered
Objective of Physiotherapy Management
- To encourage more usage of upper limb during daily activity
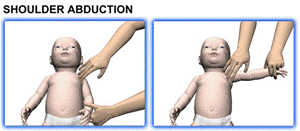
- To maintain/improve upper limb’s joint range of motion
- To increase movement ratio of corresponding upper body
- To strengthen upper limb’s muscle
- To prevent further permanent injury
- To assist/train optimum daily activity
- To improve upper limb’s joint sensation
Sign & Symptom
- Weakness of the involve upper limb
- Impaired upper limb’sjoint sensation
- Part or total paralysis
- Horner’s Syndrome
- Waiter’s tip posture
- Claw-like hand
Complication
- Limited daily functions and activities due to joint stiffness and muscle tightness
- Shoulder joint stiffness
- Muscle atrophy (muscle wasting) due to prolong immobilisation
- Shoulder and elbow joint dislocation
Treatment
- Physiotherapy
- Surgery:
- Microsurgical reconstruction
- Nerve grafts and transfers.
- Tendon transfers
- Osteotomies
- Open and arthroscopic reduction of infantile shoulder dislocations
- Parental (Family) support
Prevention
- Encourage parents to enhance the care of anaesthetic (affected) limb.
- Advice parents to avoid in lifting their baby from the armpit.
- Advice parents to avoid mishandling their baby in daily activities eg lifting, bathing and feeding.
- Advice parents to always support the affected limbs with rolling towel/pillow during sitting
- Encourage parents to continue regular positioning to prevent torticollis and head flattening
Physiotherapy Treatment
- Joint compression weight bearing on the affected upper limb to improve proprioception input.
- Upper body training
- Focus training on the affected upper limbs and encourage their active participation in such functional training
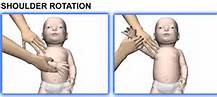
- Scapular stabilization to increase shoulder mobility
- Sensory stimulation on the affected upper limbs using various type of materials eg koosh balls, vibration and massage to increase sensory awareness
- Protective positioning of the affected upper limbs during the first week of delivery
- Active and passive exercise of the affected upper limbs
 |
 |
 |
 |
Source: images.search.yahoo.com
- Hydrotherapy (pool therapy)
- Neuromuscular re-education’ with electrical stimulation’/ Neuromuscular Electrical Stimulation’ (NMES)
Referrence
- http//membrane.com/bpp/protocol/html
- http://www.childrenshospital.org
- http://orthoinfo.aaos.org
- search.yahoo.com
- J.M.Hunter, E.J.Mackin and A.D.Callahan: Rehabilitation of the hand: surgery and therapy, 4th ed, Vol 1, 1995; 885-904.
| Last Reviewed | : | 23 August 2019 |
| Writer | : | Pauzillah binti Hj Dollah |
| Translator | : | Naqiuddin bin Mohd Johar |
| Accreditor | : | Se To Phui Lin |
| Reviewer | : | Halimah bt. Hashim |