Introduction
Herpes Simplex Virus
Herpes simplex viruses, commonly known as herpes; are categorized into two types:
- Herpes simplex type 1 (HSV-1, or oral herpes)
- Herpes simplex type 2 (HSV-2, or genital herpes).
Most commonly, herpes type 1 will cause sores around the mouth and lips. It may however, cause genital herpes.
In HSV-2, the infected person may have sores around the genitals or rectum. Although HSV-2 sores may be found in other locations, they are usually restricted to the area below the waist.
Synonyms
Herpes Simplex, Herpes
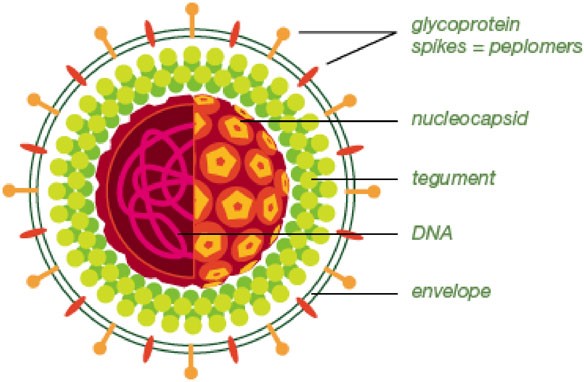
Herpes Simplex Virus Structure
Source : http://www.bio-rad.com
Oral Herpes Simplex Virus (HSV 1) Infection
Types Of HSV 1 Infection
Can be divided into 2 :
- Primary Herpes Simplex Virus (HSV 1) Infection
- Secondary or Recurrent Herpes Simplex Virus Infection
Primary HSV 1 Infection
It occurs when there is initial contact with the virus, acquired by inoculation of the mucosa, skin, and eye with infected secretions.
The virus then travels along the sensory nerve axons and establishes chronic, latent infection in the sensory ganglion (eg; Trigeminal ganglion).
Extra neuronal latency where by the HSV remains latent in cells other than neurons; such as epithelium, may play a role in recurrent lesions of lips (herpes labialis).

Vesicular Lesions Of HSV Infection On Lip
Source : www.collectionpicture.stockmd.net
Secondary HSV or recurrent HSV infection results when HSV1 is reactivated at latent sites and travels to the mucosa or skin, causing recurrent HSV infection in the form of localized vesicles or ulcers.
Prevalence
Herpes Simplex Infection is mostly subclinical and generally occurs in children and teenagers. Primary HSV infection mainly occurs in children 6 months to 5 years of age. This virus can be spread by skin-to-skin contact with an infected adult.
Primary Herpes Simplex Infection In A Baby
Source: https://pedclerk.bsd.uchicago.edu/page/mouth-infections-and-other-common-lesions
Pathogenesis
The herpes simplex infection is very contagious. It can be passed easily to other person through direct contact. Touching and sharing things with the infected person especially when the person is having active lesions can lead to HSV infection.
Most persons however, get herpes simplex from an infected individual who does not have sores. Doctors call this “asymptomatic viral shedding.” Additionally, it is possible to get genital herpes from HSV-1 if the individual has had cold sores and performed sexual activities during that time.
Primary HSV 1 Infection
Clinical manifestations
There is a 1 to 3 days viral prodromal of fever, loss of appetite, malaise and myalgia that may also be accompanied by headache and nausea. Oral pain leads to poor oral intake, and patients may require hospitalization for hydration. The disease is self-limiting in otherwise normal patients and resolves within 10-14days, typical for a viral illness.
Oral findings
- Primary Gingivostomatitis.
- Within a few days of the prodrome, erythema and clusters of vesicles and/or ulcers appear on hard palate, attached gingiva and dorsum of tongue. These are considered as keratinized epithelium. It may also affect non-keratized epithelium which are buccal and labial mucosa, ventral tongue and soft palate.
- Vesicles break down to form ulcers that usually 1-5mm wide and coalesce to form larger ulcers.
- Gingiva is often fiery red and mouth is extremely painful, causing difficulty in eating.
- Pharyngitis, which usually found in adult, will cause swallowing difficulties.

Herpetic Gingivostomatitis
Source: http://www.aafp.org/afp/2010/1101/p1075.html
Vesicular Lesions Of HSV Infection On Palate
Source: http://intranet.tdmu.edu.ua
Secondary HSV 1 Infection
People who are infected with HSV will have the virus for the rest of their lives. Even if it asymptomatic, the virus will continue to live in an infected person’s nerve cells. Some people may experience regular outbreaks. Others will only experience one outbreak, after which the virus may become dormant.
Reactivation of HSV1 can be cause by a few factors:
- Stress
- Menstrual periods
- Fever or illness
- Strong sunlight exposure or sunburn
- Surgery
- Immunocompromised (e.g : HIV, undergone organ transplantation, chemotherapy, leukaemia)
Clinical manifestations
Oral findings are as in primary HSV1 infection. In immunocompromised patients; intraoral recurrent HSV ulcers may appear different, the size may be larger and it takes longer time to heal and disseminate to other sites, if undiagnosed or untreated.
Site
Most blisters of Oral herpes (HSV-1) appear on the lips or around the mouth and is called herpes labialis. Sometimes blisters form on the face or on the tongue, however they can appear anywhere on the skin.

Herpes Labialis In Adult
Source: http://youritablets.com/herpes-type-2/
Some medical or dental practitioners and nurses may develop infection around the fingers (if gloves are note used) due to direct contact with the active source of infection. This is called herpetic whitlow.

Herpetic Whitlow
Source: http://diseasespictures.com/herpetic-whitlow/
Sign And Symptoms
- Tingling, itching, or burning sensation for a day or so before the blisters appear.
- Sores: Painful and fluid-filled blisters may appear. Blisters break and often ooze fluid forming a crust before healing. The sores appear between 2 and 20 days after exposure to the virus.
- Flu-like symptoms. Fever, muscle aches, or swollen lymph nodes in the neck
- An eye infection (herpes keratitis). Sometimes the herpes simplex virus can spread to one or both eyes. If this happens, pain, sensitivity to light, fluid discharge and a gritty feeling in the eye/s may be experienced. Scarring of the eye may result without prompt treatment leading to cloudy vision and even loss of vision.
Diagnosis
Clinical presentation is usually sufficient to diagnose HSV infection.
However, there are several lab procedures that can be done to confirm the diagnosis of HSV infection.
- Serologic test for HSV antibodies.
- Viral culture
- Detection of HSV antigen by DFA test
- Tzank smears: prepared slides are stained with Wright Giemsa stain, followed by light microscopy examination.
- HSV DNA detection using PCR
Treatment
Currently there is no cure for this virus. Treatment therefore focuses on symptomatic relief.
It is possible that the sores will disappear without treatment. However, the following medications may help reduce the frequency and severity of the recurrence and limit outbreaks:
- Acyclovir
- Famciclovir
- Valacyclovir
These medications may come in pills form (oral), or may be applied as cream. For severe outbreaks, these medications may also be administered parenterally (injection).
Other symptomatic medications are anti-inflammatory drugs, anti-pyrexia and analgesics.
Conclusion
Herpes, though is NOT life-threatening, it can be life-changing. It is important to know about HSV; the risk factors that can lead to the viral infection, how to prevent it from spreading and recurring in infected person.
References
- Vesiculo-bullous lesions of the oral mucosa. S.R Prabu. Textbook of Oral Medicine, Oxford University Press; 2004.
- Oral and Maxillofacial Pathology. Neville and Damm. Second edition; 2005.
- The laboratory diagnosis of herpes simplex virus infections. Singh A, Preiksaitis J, Ferenczy A, Romanowski B; Can J Infect Dis Med Microbiol 16(2): 92-98, 2005.
| Last Reviewed | : | 6 May 2016 |
| Writer / Translator | : | Dr. Hartinie bt. Muhamad |
| Accreditor | : | Dr. Hans Prakash a/l Sathasivam |