Introduction
Leukoplakia was first defined by World Health Organisation in 1978 as a white patch or plaque that cannot be characterized clinically or pathologically as any other specific disease1. Leukoplakia is thus a clinical diagnosis and a definitive diagnosis can only be made by eliminating suspected etiological factors. It is a potentially malignant disorder of oral mucosa.
Considering the risk of malignant transformation of leukoplakia, in 2005 the WHO working group has amended the earlier definition of leukoplakia, to stand as ‘white plaques of questionable risk having excluded other known diseases or disorders that carry no increased risk for cancer’1.
Leukoplakia is categorized into two types, based on the clinical appearance:
- Homogenous leukoplakia: The most common type, are uniformly, well demarcated white plaques which can vary from smooth thin surface to a velvety appearance with fissures. Sometimes lesions are wide-spread.
- Non-homogenous leukoplakia: This type may be nodular, verrucous and speckled leukoplakia which consists of white nodules or plaque intermixed with red, often eroded area of mucosa. When combined with reddish area, they are also called erythroleukoplakia.
Synonyms
Oral leukoplakia (also termed leucoplakia, leukokeratosis, leukoplasia, idiopathic leukoplakia, idiopathic keratosis, or idiopathic white patch)
Etiology
The actual cause remain unknown however there are hypotheses that oral leukoplakia occurrence are related to these factors;
- Tobacco smoking: researchers have shown that 80% of patients are with this habit.
- Alcohol: seems to give synergistic effect with tobacco for development of oral cancer from oral leukoplakia but not the occurrence of leukoplakia itself.
- Sanguinaria : some toothpaste or mouth rinse containing this herbal extract may cause development of leukoplakia in the users’ mouth
- Ultraviolet radiation: is a causative factor for the leukoplakia of the lower lip vermilion especially in an immunocompromised person.
- Microorganism :
- Candida albicans : fungal organism that can colonize the superficial layers of the oral mucosa which may produce hyperplastic and dysplastic changes in the epithelial lining. Clinically it looks as a thick granular plaque with mixed white and red coloration and is termed as candida leukoplakia or candidal hyperplasia.
- Human Papillomavirus (HPV) subtypes 16 and 18 have been identified in some leukoplakias.
- Trauma: chronic mechanical irritation can produce a white lesion similar to true leukoplakia, termed as frictional keratosis which is readily reversible after elimination of the trauma.
Pathogenesis
Oral leukoplakia development as premalignant lesions involves different genetic events. Activation of oncogenes deletion and injuries to suppressor genes and genes responsible for DNA repair will contribute to a defective functioning of the genome that governs the cell division. These will lead to a series of mutation and a malignant transformation will occur. For example, tobacco smoking may induce hyperkeratinization, with the potential to revert following cessation, but at some stage, mutations will lead to unrestrained proliferation and cell division.
Oral Leukoplakia
Clinical features
Age
Occurs predominantly in the middle-aged and elderly, mostly in patients older than 40 years
Gender
Occurs more in men than women
Oral findings
Vary in size: some are small and focal, others more widespread, involving very large areas of oral mucosa. In other patients, several discrete separate areas of leukoplakia can be seen.
Clinical presentations of leukoplakia could be from homogenous white plaques, which can be faintly white or very thick and opaque, to nodular white lesions, or lesions admixed with red lesions.
Uniformly demarcated red area of oral mucosa that cannot be characterized as any other definable lesions is called erythroplakia.
Site
About 70% of oral leukoplakia are found on lip vermilion, buccal mucosa and gingiva. Other site would be floor of mouth and tongue which has the higher risk of malignant change.
Clinical appearance
Early lesions may present as slightly elevated gray or gray white plaques which may appear translucent, fissured or wrinkled and are typically soft and flat. This type may disappear or remain unchanged.
When risk habits are continuous, example in smokers, the affected site may slowly extend, become thicker, leathery and more numerous. Some may regress but some may become more severe with increased surface irregularities. At this stage, the leukoplakia may be called granular, nodular or verrucous/verruciform leukoplakia.
Proliferative leukoplakia (PVL) is a special high risk form of leukoplakia, characterized by development of multiple keratotic plaques with roughened surface. PVL rarely regress despite therapy, having strong predilection towards women and low association with tobacco use.
Some leukoplakia might have scattered patches of redness, this type is called erythroleukoplakia or speckled leukoplakia.
Homogenous Oral Leukoplakia

Widespread, flat and thin, white plaque of homogenous leukoplakia
Picture: van der Waal I. http://www.medicinaoral.com/mcdoralfrcc01/v20i6/mcdoralv20i6p685.pdf
Well demarcated wrinkled white plaque of homogenous leukoplakia
Picture: Juniordentist.com

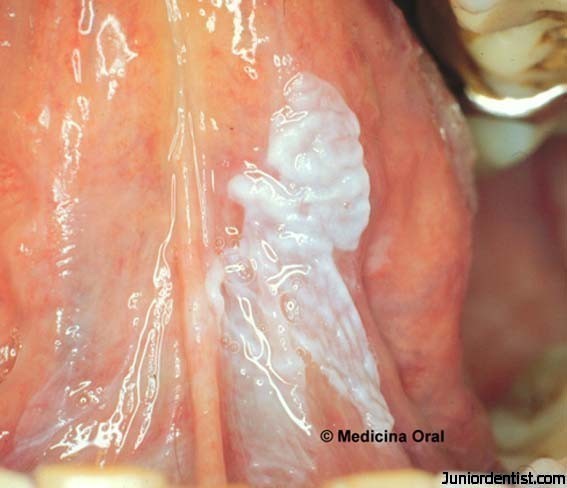
Velvety or corrugated appearance of homogenous leukoplakia
Picture: Juniordentist.com
Non-Homogenous Oral Leukoplakia

Non-homogenous nodular leukoplakia
Picture: van der Waal I. http://www.medicinaoral.com/mcdoralfrcc01/v20i6/mcdoralv20i6p685.pdf

non-homogenous granular leukoplakia
Picture: oral pathology quizlet

Erytroleukoplakia : a mixture of reddish area with white plaque
Picture: pocketdentistry.com

Proliferative verrucous leukoplakia
Picture: emedicine.medscape.com

Non-homogenous verruciform leukoplakia
Picture: www.oralpath.co.uk
Diagnosis
The provisional diagnosis of leukoplakia is based on clinical observation of a white patch that is not explained by a definable cause, such as trauma.
Malignant Potential
The malignant potential of leukoplakia depends on the appearance, site and some etiological factors. The prevalence of malignant transformation in leukoplakias is 2-35% over 10 years.
- Appearance
- Homogenous leukoplakia: most common in buccal mucosa, uniformly white plaques, are usually of low malignant potential.
- Non-homogenous leukoplakia: nodular, granular, verrucous and speckled leukoplakia has a high risk of malignant transformation.
- Site
- The high risk sites for malignant transformation include the ventrolateral tongue surface and floor of mouth.
- Etiological factors
- Human papilloma virus often associated with the special high risk type of leukoplakia i.e proliferative verrucous leukoplakia; a diffuse white plaque or papillary white lesion.
- Chronic candidal infection is common in speckled leukoplakia; they may induce dysplasia in the epithelium of the leukoplakia and increase risk of malignant potential.
- Syphilitic leukoplakia especially on dorsum of tongue, is a feature of tertiary syphilis which rarely seen now, but the malignant potential is high
Diagnosis
There are no clinical signs or symptoms which reliably predict whether a leukoplakia will undergo malignant change; thus there must be use of microscopy to detect dysplasia. Biopsy is therefore mandatory for those leukoplakias which are:
- In patients with history or concurrent head and neck cancer
- Non-homogenous leukoplakia; with red areas, verrucous and indurated.
- High risk site
- Without obvious etiological factors
Management
Leukoplakia may undergo spontaneous remission; however some may be potentially malignant and become cancerous. Thus both behavior modification and active treatment of the lesion are indicated. Patient information is an important aspect in management of leukoplakia.
- Removal of known risk factors (tobacco, alcohol and trauma) is a mandatory first step.
- Patients with discrete and homogenous leukoplakia should be re-examined 2-3 months after instituting the factors. If the lesion persists, it should be removed.
- Many patients with leukoplakias belong to lower socio-economic groups whom may not always accept or understand the need to re-attend. Therefore many suggest removing the lesion in the early visit.
- A definitive histopathologic diagnosis will guide the course of treatment, therefore a biopsy is mandatory in non-homogenous leukoplakia; speckled, verrucous or at high-risk site.
- BIOPSY: Tissue obtained for biopsy, should be taken from clinically most severe area, multiple biopsies of large or from multiple lesions may be required.
- SURGERY: Complete removal should be done for patients diagnosed with moderate or severe dysplasia.
- ELECTROCAUTERY and CRYOSURGERY: for large and multiple sites leukoplakia or patients who are contraindicated for surgical procedures.
- LASER EXCISION (carbon dioxide laser): may have advantage over the use of scalpel, as intraoperative bleeding and the need for mucosal flaps are reduced.
- Follow-up is extremely important: patients should be regularly checked at 3, 6, and 12 months for any: size change, appearance of red lesions, ulceration, recurrences and new lesions.
Conclusion
No clinical or histological characteristics are able to reliably predict potential malignancy in leukoplakia; therefore treat predisposing factors, stop risk habits and surgically remove discrete lesions and those with moderate or severe dysplasia.
References
- J Oral Pathol Med ; Nomenclature and classification of potentially malignant disorders of the oral mucosa. S.Warnakulasuriya, Newell.W.Johnson, I.van der Wall: 2007;36:575-80.
- Oral and Maxillofacial Pathology. Neville and Damm. Second edition; 2005
- Oral and Maxillofacial medicine. Crispian Scully CBE. First edition; 2004
- Oral Medicine . Burket’s. Eleventh edition; 2008
| Last Reviewed | : | 30 June 2016 |
| Writer | : | Dr. Hartinie bt. Muhamad |
| Accreditor | : | Dr. Ajura bt. Abdul Jalil |







