Chemo-Radiotherapy – Induced Oral Mucositis
Introduction
Oral mucositis is inflammation of the oral mucosa resulting from chemotherapy or radiation therapy in the treatment of cancer. It typically presents as erythema or ulcerations of the oral mucosa. When high dose chemotherapy is used such as in hematopoietic stem cell transplantation (HSCT) cases, both the oral and gastrointestinal (GI) tract mucositis may occur. Studies have shown that alimentary tract mucositis can affect the planned cancer treatment schedule leading to prolong hospital stay, increases mortality and morbidity and contributes to rising health care costs.
Generally, only 5 to 15% of patients who underwent chemotherapy for cancer treatment get either oral or GI mucositis or both. However, the incidence and severity differs with different type of chemotherapy agents used. For example, melphalan a widely used agent for bone marrow transplantation affect about 80% of patients with more than half suffering from severe grade of oral mucositis. With many other chemotherapy agents, the oral mucositis is usually mild to moderate in severity.
Radiotherapy to the head and neck is associated with severe grade of oral or GI mucositis in more than 50% of patients. Fractionated radiation therapy has been reported to increase the risk of mucositis to more than 70% of patients. Oral mucositis is particularly profound and prolonged among HSCT recipients who receive total-body irradiation and concomitant chemotherapy.
Signs and symptoms of oral mucositis
Cancer patients undergoing chemotherapy usually become symptomatic four to five days after beginning treatment, reaching a peak at around day 10, and then slowly improving over the course of a few weeks. On the other hand mucositis associated with radiotherapy usually appears at the end of the second week of treatment and may last for six to eight weeks after completion of treatment.
The symptoms and signs experienced by patients are due to cell death of mucosal lining of the mouth in reaction to chemo- or radiation therapy. Mucositis can present clinically as:
- Red patches
- Ulcers of varying sizes ranging from 0.5 cm to greater than 4 cm
- And can be severely painful affecting speech, eating, or even mouth opening, as well as loss of taste


Figures show severe oral ulcerations that are painful and affect oral functions (adapted from www.diseasepicture.com)
Pathophysiology of Mucositis
The pathophysiology of mucositis can be divided into its 5 stages:
- Initiation phase
- Message generation phase
- Signalling and amplification phase
- Ulceration phase
- Healing phase
Different cytokines are responsible for the various stages. The initiation phase is caused by the production of free radicals caused by the chemo- or radio- therapy, which damages cell DNA. This causes the production of cell transcription factors such as NF-?B, which up regulates inflammatory cytokines, marking the beginning of the ulceration phase. Main inflammatory cytokines involved are IL-1 and TNF-alpha. During the healing phase, epithelial cells are attracted to the site of the ulcer and begin the re-epithelialization of the ulcers.
Diagnosis and grading of Mucositis
Diagnosis is based on the symptoms the patient is experiencing and the appearance of the tissues of the mouth following chemotherapy or radiotherapy. Erythematous burn-like sores or ulcers throughout the mouth is enough to diagnose mucositis. The severity of oral mucositis can be evaluated using several different assessment tools. One of the most commonly used is the World Health Organization (WHO) Oral Toxicity score. This system combines the mucosal changes and oral functions.
The WHO Oral Toxicity Scale
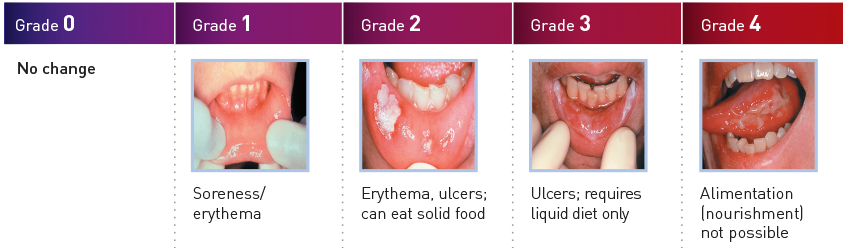
Adapted from www.mugard.com
Management of Oral Mucositis
There is currently no single specific treatment that is effective to manage mucositis. Most treatments aim on reducing the mucositis severity and adverse effect. The general approaches include the following:
- Effective oral care
- Dietary modifications
- Topical mucosal protectants
- Appropriate use of topical anaesthetics
- Systemic analgesics
Management of oral mucositis begins with patient education and reinforcing the importance of good oral care throughout cancer treatment. Since mucositis is self-limiting, the goal of treatment is to make the patient as comfortable as possible and to maintain adequate nutrition and prevent dehydration. In both inpatient and outpatient settings, patients should be assessed routinely to ensure good symptom control and maintaining of general health.
Generally, management of mucositis can be divided into 5 main approaches, including the following:
-
Oral debridement
Maintaining oral hygiene must be done in cautious manner. Patients undergoing chemotherapy frequently become neutropenic and thrombocytopenic. Normal tooth brushing can cause gingival bleeding and, more importantly, result in transient bacteraemia. In severe cases, where tooth brushing is not possible, frequent rinsing with several types of rinsing solution may be helpful. Dried secretions may become hardened on the mucosal surfaces, particularly the palate and often misdiagnosed as candidiasis by inexperience clinicians. Saline or sodium bicarbonate rinse may be used to soften and dislodge them. Sometimes mucolytic agent, such as Alkalol can be used to soften and dislodge them.
- Oral decontamination
Studies show that antiseptic rinsing with chlorhexidine is effective in reducing the overall bacterial load in the oral cavity. Candidal prophylaxis if advocated usually includes nystatin rinses. Fluconazole may be used for candidal prophylaxis or for treatment of suspected candidiasis in immunocompromised patients. In some centres, antiviral are also use to prevent herpes simplex virus (HSV) reactivation in susceptible patients. However, none of these treatments has been shown to specifically reduce the risk of developing oral mucositis.
-
Topical and systemic pain management
Pain in patients with oral mucositis can be well controlled by several types of topical rinses. In many cases, 2% viscous lidocaine, magic mouthwash preparations, and topical morphine solution are adequate in controlling the pain. In severe cases, systemic analgesics may be used together to achieve adequate pain control. Topical solutions should be kept in the mouth from 2-5 minutes, or as tolerated. Frequent rinsing with sodium bicarbonate solution helps to keep the mucosa moist, reduces caking of secretions, and soothes inflamed or ulcerated mucosa. Several newly developed topical mouth rinse for reducing mucositis are now available in the market; namely Palifermin, Gelclair, NeutraSal, Episil and many others.
- Prophylaxis / prevention
Cryotherapy with ice chips has been shown to effectively attenuate the onset and severity of mucositis in patients undergoing bolus chemotherapy with 5-fluorouracil and melphalan. Patients should suck on ice chips for 30 minutes prior to and during the chemotherapy infusion.
- Control of bleeding
Maintaining platelets at least 20,000 cells/µL and using topical thrombin packs and topical anti-fibrinolytic agents, such as tranexamic acid, may control bleeding from ulcers.
Available medications for alleviating mucositis and their function:
- Palifermin is a human KGF (keratinocyte growth factor) that has shown to enhance epithelial cell proliferation, differentiation, and migration
- Cytokines and modifiers of inflammation (e.g., IL-1, IL-11, TGF-beta3)
- Amino acid supplementation (e.g., glutamine),vitamins, and colony-stimulating factors
- Gelclair: a barrier protection agent
- MuGard: muco-adhesive oral protectant that is designed to form a protective hydrogel coating over the oral mucosa while a patient is undergoing chemotherapy and/or radiotherapy cancer treatments
- NeutraSal is an FDA-cleared calcium phosphate mouth rinse
- Episil oral liquid: creates a lipid membrane that mechanically bonds to the oral cavity mucosa to coat and soothe inflammation and ulcerations, and blanket painful lesions
- Water based Hydroxypropyl methylcellulose film-forming agents (e.g. Zilactin) act as lubricant and mucosal barrier.
Guidelines
Comprehensive, evidence-based guidelines for the prevention and treatment of oral mucositis are available:
- Mucositis Guidelines Leadership Group of the Multinational Association of Supportive Care in Cancer and International Society of Oral Oncology (MASCC/ISOO)
- Oncology National Comprehensive Cancer Network – NCCN Task Force Report: Prevention and Management of Mucositis in Cancer Care
Complications
Sores or ulcerations can become infected by virus, bacteria or fungus. Pain and loss of taste perception makes it more difficult to eat, which leads to weight loss. Ulcers may act as a site for local infection and a portal of entry for oral flora that, in some instances, may cause septicaemia (especially in immunosuppressed patients). Approximately half of all patients who receive chemotherapy develop such severe oral mucositis that becomes dose-limiting such that the patient’s cancer treatment must be modified, compromising the prognosis.
Some Tips for Managing Mucositis
Mucositis can be alleviated at home with the following tips:
- Drink 8 glasses of water daily (about 2 litres). Purified or deionized water can reduce irritation.
- Drink sports drinks with electrolytes, such as Gatorade or Powerade, to stay hydrated if indicated
- Cut down on or avoid caffeine and alcohol since they can dry out and further irritate tissue
- Eat soft comfort foods like ice cream, popsicles, milkshakes, smoothies, pudding, yogurt, gelatin, mashed potatoes, bananas and non-spiced applesauce
- Avoid acidic foods and drinks that irritate tissues such as citrus fruits and juices, tomatoes, spicy or salty foods and even carbonated drinks. Also avoid hot peppers, curry, salsa, and raw ginger and onions until you feel better.
- Avoid all forms of tobacco and nicotine because these irritate raw tissues like mouth sores and delay healing.
- Avoid foods and liquids that contain a lot of sugar.
- Use lip balm for dry lips and avoid breathing through your mouth.
- Water based lubricant may be used if dry mouth present
- If you wear dentures, use them only for meals to let your gums rest and to reduce irritation.
- Use a very soft toothbrush and floss gently, to avoid irritating your gums.
References
- Rubenstein EB, et al. Clinical practice guidelines for the prevention and treatment of cancer therapy-induced oral and gastrointestinal mucositis. Cancer. 1 May 2004; 100(9 Suppl.):2026-46.
- Rubenstein EB, et al. Evidence-based guidelines for the Multinational Association of Supportive Care in Cancer and the International Society for Oral Oncology.
- National Cancer Institute Common Toxicity Criteria. Version 2.0, June 1, 1999
- Sonis S, Clark J. Prevention and management of oral mucositis induced by antineoplastic therapy. Oncology 1991; 5:11-18.
- McGuire DB, Altomonte V, Peterson DE et al. Patterns of mucositis and pain in patients receiving preparative chemotherapy and bone marrow transplantations. Oncol Nurs Forum 1993; 20:1493-1502.
- Guggenheimer J, Verbin RS, Apple BN et al. Clinco-pathologic effects of cancer chemotherapeutic agents on human buccal mucosa. Oral Surg Oral Med Oral Pathol 1997; 44:58-63.
- Wilkes JD. Prevention and treatment of oral mucositis following cancer chemotherapy. Semin Oncol 1998; 25:538-551.
| Last Reviewed | : | 26 October 2016 |
| Writer | : | Dr. Abdul Rahim bin Ahmad |
| Accreditor | : | Dr. George Boey Teik Foo |







