Introduction
Osteoporotic fractures are emerging as a major public health problem in the aging population. Fractures result in increased morbidity, mortality and health care expenditures. At 50 years of age, 4 in 10 women will experience a hip, vertebral or forearm fracture in their remaining lifetime, and are more likely to die from complications of fracture than from breast cancer1.
Although osteoporosis is frequently considered to be a disease of elderly women, men account for 30% of hip fractures worldwide and mortality after such fractures are greater in men than in women. Increased mortality, pain, disability, depression and loss of independence have been well documented after hip and vertebral fractures.
Due to the high risk of morbidity and mortality after an osteoporotic fracture, older adults require an interdisciplinary approach to their care. In particular, attention must be given to the prevention of common fracture complications, rehabilitation, assessment of the cause of fracture, and prevention of subsequent fractures.
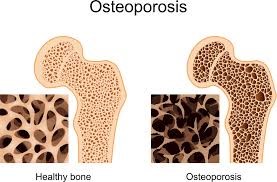
Definition
Osteoporotic fractures (fragility) are defined as fractures associated with low bone mineral density (BMD) and include clinical spine, forearm, hip and shoulder fractures which result from mechanical forces that would not ordinarily result in fracture.
Essential For Prevention
Advanced age is the most important factor in that it is associated with not only reduced bone mass but also reduced in the quality of the bone. Thus, for any given bone mass, the risk of fracture increases with age.
Osteoporotic fragility fractures can cause substantial pain and severe disability, often leading to a reduced quality of life. Hip and vertebral fractures are associated with decreased life expectancy.
Hip fracture nearly always requires hospitalization, is fatal in 20% of cases and permanently disables 50% of those affected; only 30% of patients fully recover. Only one in three vertebral fractures is diagnosed. One vertebral fracture increases a patient’s risk of sustaining another vertebral fracture fivefold, 20% of these within a year.
Steps To Prevention
Non-pharmacological prevention of osteoporotic fractures includes :
- Weight-bearing exercise in sedentary individuals. Exercise can reduce the risk of falls when designed to improve balance and increase lower extremity strength.
- Screening and identification of low bone mass in individuals who have:
- Parental history of hip fracture.
- Alcohol intake of four or more units per day.
- Rheumatoid arthritis.
- Female gender.
- Corticosteroid therapy or Cushing’s syndrome.
- Ankylosing spondylitis.
- Crohn’s disease.
- Untreated premature menopause (<45 years) or prolonged secondary amenorrhoea.
- Low body mass (<19 kg/m2) and anorexia nervosa.
- Poor diet (particularly if calcium-deficient) or malabsorption syndromes, eg: coeliac disease.
- Prolonged immobilization or a very sedentary lifestyle.
- Smoking.
- Primary hypogonadism (men and women).
- Primary hyperparathyroidism.
- Hyperthyroidism.
- Osteogenesis imperfecta.
- Caucasian or Asian origin.
- Post-transplantation.
- Chronic renal failure.
- Identifications of risk factors for fall in persons with low bone mineral density or other major risk factors for osteoporotic fractures (e.g. prior minimal trauma fracture, low body weight, loss of 2 or more inches of height)
-
Predictors of fall related to hip fractures:
- Increased height
- Lower extremity muscle weakness/atrophy
- Poor visual acuity
- Neurodegenerative disorders of the central nervous system
- Postural instability
- Medications affecting postural stability
- Approaches to reduce the impact force of the fall.
- lowering bed height and the use of foam mats beside the bed
- the use of external hip protectors to minimize the impact force of a fall on the hip in frail elderly
- Reduce polypharmacy, especially sedative medications.
Pharmacological prevention
The primary goal of therapy is to reduce the risk of osteoporotic fractures based on T-score in BMD screening and the presence of other factors that may contribute to the risk of osteoporosis and osteoporotic fractures. The treatment includes:
- Calcium & vitamin D. Total intake 800-25 000 units/day equal to 2 glass of milk per day
- Hormone therapy 0.625 mg CEE (1-2 mg estradiol)
- Bisphosphonates i.e. Alendronate (Fosamax) 70mg/wk.
Bisphosphonates are more potent antiresorptive agents, effective in the prevention of both vertebral and nonvertebral fractures and are recommended for the treatment of high-risk patients. If bisphosphonates are unsuitable then calcitriol may be considered.
References
- Cathleen S., Colón-Emeric and Saag, K.G. (2006). Osteoporotic fractures in older adults. Best Pract Res Clin Rheumatol, 20(4): 695–706.
- www. sci-hub.com
- Wilkins, C.H., & Birge, S.J. Prevention of osteoporotic fractures in the elderly.
- A National Clinical Guidelines. (2005). Management of osteoporosis and the prevention of fragility fractures.
- National Osteoporosis Guideline Group. (2004). Guideline for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK.
| Last Reviewed | : | 7 November 2016 |
| Writer | : | Dr. Siti Aishah bt. Johari |
| Accreditor | : | Dr. Ruziaton bt. Hasim |







