Periodontitis (Periodontal disease/gum disease) is an inflammatory disease affecting the periodontal tissues (tissues that surround and support the teeth). Periodontitis involves the progressive loss of alveolar bone around the teeth; if left untreated, this can lead to the loosening and subsequent loss of teeth. Periodontitis is also more common in adults. The loss of periodontal attachment increases with age, which then leads to tooth migration due to inability of teeth to resist soft tissue and biting forces (Ong MA et al,1998).
Orthodontic treatment(braces) is usually carried out to correct malocclusions which include jaw discrepancies as well as malalignment of teeth. This treatment modality not only improves one’s facial aesthetics, but, also aids in better mastication and speech, thereby contributing to improved general and oral health as well as self- esteem. (Samah A et al.,2014).
There is a vital relationship between periodontal disease and orthodontic treatment. A healthy periodontal tissue is important in order to ensure good orthodontic treatment outcome, whilst, orthodontic treatment may help to improve the overall aesthetic and functional rehabilitation of a periodontally compromised dentition (Gkantidis N et al, 2010).The available evidence also seem to suggest a strong correlation between presence of malocclusion and periodontal disease but does not necessarily mean that malocclusion is the cause of periodontitis (Bowen A-M, 2008).
Healthy / normal Periodontal Tissue Response to Orthodontic Forces
Orthodontic tooth movement occurs through application of controlled forces on teeth and consequent remodeling of bone. Bone surrounding a tooth which is subjected to an orthodontic force responds in the following manner: resorption occurs where there is pressure and new bone forms where there is tension (Figure 1) (Kitaura H et al., 2014). This “frontal resorption” occurs when light forces are applied. However, when excessive pressure is applied to a tooth, there is some tooth movement initially; whereby, the periodontal ligament is compressed, until the blood supply is cut off from the periodontal ligament. This creates an avascular cell-free zone called “hyalinization” and tooth movement then stops temporarily. The hyalinized zone has to be removed by periodontal ligament regeneration before tooth movement can then resume. In this instance, the adjacent alveolar bone undergoes “undermining resorption”. Frontal resorption of bone is more desirable than undermining resorption, causes less discomfort and is least harmful to the periodontium.
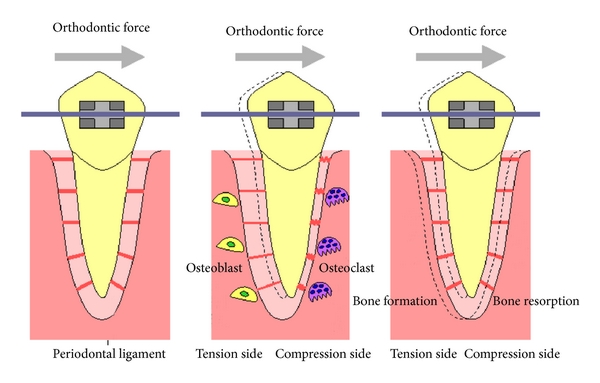
Figure 1
Unhealthy / diseased Periodontal Tissue Response to Orthodontic Forces
In subjects with periodontitis, the periodontal ligament does not regenerate when there is inflammation in the periodontal tissues. When teeth are moved orthodontically, in the presence of plaque, this force can cause bone and attachment loss (Ong MA et al;1998) and there is a significantly higher loss of bone density in subjects with periodontitis compared with normal subjects. (Zhi-Gui Ma et al, 2015).
Orthodontic components which are attached to the tooth surface may also hinder effective cleaning of teeth. This will lead to further accumulation of plaque and increase the risk for periodontal disease. Those patients who have a pre-existing periodontal disease have a higher risk of their periodontal health deteriorating further if plaque control is inadequate (Ong MA et al.,1998).
However this doesn’t mean that the patient with compromised periodontal tissues cannot benefit from orthodontic treatment. It simply means their periodontitis needs to be controlled first before, during and after the entire orthodontic treatment (Gkantidis N et al., 2010).
How can orthodontic treatment help those with compromised periodontal tissue?
The loss of periodontal support may lead to the migration of a single tooth or a group of teeth which will eventually cause tipping/proclination, rotation, over-eruption, spacing, loss of teeth or traumatic bite (figure 2) (Ong MA et al., 1998). These conditions, not only impair function and aesthetics but also reduce the success rate of periodontal treatment as patient finds it hard to maintain good oral hygiene.
Orthodontic treatment (braces) can be used to improve the aesthetics, function and periodontal health of a person’s dentition. Properly aligned teeth are easier to clean and promote healthier periodontal tissue. Some studies have found that there is improvement of the periodontium due to less plaque accumulation on the orthodontically uprighted teeth(Ong MA et al.,1998). A systematic review concluded that subjects with malocclusion have worse periodontal health than those without malocclusion. However, there is a lack of evidence to suggest that orthodontic treatment may prevent periodontal problems (Bollen A-M,2008).
Orthodontics can be an adjunct treatment to improve periodontal health by:
- Uprighting or repositioning of abutment teeth prior to restorations or implant placement
- Space creation or reduction/closure to facilitate prosthetic replacement of teeth
- Correcting cross-bites which are causing bite interference
- Extruding or intruding teeth to facilitate restorative work
- Correcting crowding of teeth
- Restoring lost vertical dimension
- Increasing or decreasing overjet/overbite
- Closure of spaces in between teeth
(Ong MA et al.,1998)
 |
 |
 |
|
What is the risk for patient with periodontal disease receiving orthodontic treatment?
The most important factor in the initiation, progression and recurrence of periodontal disease in reduced periodontal tissue is the presence of microbial plaque. In healthy reduced periodontal tissue support regions, orthodontic forces kept within biological limits do not cause gum inflammation. Clinical studies have demonstrated that with plaque control, teeth with reduced periodontal support can undergo successful tooth movement without compromising their periodontal situation (Ong MA et al.,1998).
However, orthodontic brackets and elastics might interfere with effective removal of dental plaque; affect the equilibrium of oral microflora by increasing bacteria retention, thereby increasing the risk of periodontitis (figure 3). Regeneration of periodontal tissues is also hampered by presence of inflammation in the periodontal tissues. Orthodontic forces on teeth may increase their mobility due to further bone loss and root resorption in susceptible patients. The periodontal complications associated with orthodontic therapy mainly include gingivitis, periodontitis, gum recession or hypertrophy, alveolar bone loss, dehiscences, fenestrations, interdental fold, and dark triangles. Bone loss in patients with periodontitis has been shown to be greater than in those with normal periodontal tissue (Gkantidis N et al.,2010).
Risk factor sfor periodontal destruction during orthodontic treatment.
- Long treatment duration
- Increased amount of tooth movement
- High force magnitude and over longer duration
- Extractions of teeth and large spaces to close during treatment
- Poorly controlled or active periodontal disease, made worse if medically compromised, eg. Diabetes Mellitus
- Inadequate/ineffective cleaning of teeth

Figure 3
What are the measures to be taken when treating patients with periodontal disease?
Orthodontic treatment is usually contraindicated in patients with active periodontal disease, as the chance of further periodontal deterioration is high in such cases. It is generally recommended to start orthodontics treatment after a complete periodontal therapy to ensure there is no further breakdown of periodontal tissues.
- Before orthodontic treatment
A thorough assessment of the periodontal health and a reasonably good level of attached gum are recommended prior to the orthodontic treatment (Samah A et al., 2014). However, teeth with reduced periodontal support can be safely moved provided there is adequate plaque control. Therefore, the initial management has to include stabilization of the periodontal condition of the affected teeth. Scaling, root planning and or any other periodontal treatment should be performed as appropriate before any tooth movement is undertaken. However the major periodontal treatment, for example, bone modification surgery ought to be delayed until the end of orthodontic treatment, because tooth movement may modify gum and bone morphology (GoldmanHM and Cowen DW, 1968).
Once the periodontal disease has been fully stabilized and the patient is able to maintain a good standard of oral hygiene, orthodontic treatment can begin. It is suggested to allow 2–6 months from the end of periodontal therapy until orthodontic appliance placement, for periodontal tissue remodeling, restoration of health and reevaluation of patient’s complaint (Gkantidis N et al.,2010).
- During orthodontic treatment
Orthodontic treatment aims at providing an acceptable functional and aesthetic occlusion with appropriate tooth movements. Fixed appliance treatment usually is needed (figure 4)

 Before treatmentHalf way through fixed appliance treatment
Before treatmentHalf way through fixed appliance treatment
 Before treatmentAfter fixed appliance treatmentFigure 4
Before treatmentAfter fixed appliance treatmentFigure 4Patients with stabilized reduced periodontal tissue may be susceptible to periodontal disease again. Therefore during orthodontic treatment, professional cleaning and examination of periodontal tissues should be performed routinely. Close monitoring and support is mandatory for these patients; if the patient fails to maintain high level of oral hygiene, orthodontic treatment should be interrupted. (Laura Mitchell 2013, Ong MA et al.,1998, Gkantidis N et al.,2010).
Treatment should be performed with the simplest possible orthodontic systems (simple alignment and space closing) to avoid circumstances that favor increased dental plaque accumulation (figure 5). Patient might have to accept compromised or limit treatment objectives if necessary to avoid prolonged treatment. Besides, lighter forces should be used during treatment, due to the reduced periodontal support (Ong MA et al.,1998).

 Before treatmentAfter treatmentFigure 5
Before treatmentAfter treatmentFigure 5
(an example showing simple orthodontic treatment and compromised result)
- After orthodontic treatment
There is a high possibility that the patient’s teeth with reduced periodontal tissue will relapse later (space reopening, and teeth migration). In order to avoid this complication, permanent retentionis usually required, in the form of bonded retainers to provide additional support to periodontally involved teeth (figure 6). The patient must be taught how to maintain excellent oral hygiene around these retainers. For patients with loss of teeth and/or occlusal trauma, retention should be accomplished by prosthetic reconstruction such as denture, bridge or implants (Gkantidis N et al.,2010).
Elective periodontal treatment or surgery should be implemented during the final stages of orthodontic treatment or even later, when the final position of teeth and supporting structures can be safely determined.
Once the orthodontic treatment is over, the patient should receive renewed oral hygiene instructions for reducing the risk of gum recession, as plaque removal and tooth cleaning will be more easily performed. In addition, patients should be introduced to a programme of regular follow-up visits to the periodontist and the orthodontist to allow close monitoring of his teeth and periodontal health (Gkantidis N et al.,2010).

 Figure 6
Figure 6
(examples of fixed retainer)
|
Orthodontic treatment of patient with periodontal disease |
|
|
Before treatment |
|
|
During treatment |
|
|
After treatment |
|
Conclusion
Periodontal health is an essential requirement for any kind of dental treatment. Orthodontic treatment along with good patient compliance and absence of periodontal inflammation can provide satisfactory results without causing irreversible damage to teeth and periodontal tissues. Furthermore, orthodontic treatment can expand the possibilities of periodontal therapy in certain patients, contributing to better control of plaque accumulation and improving the overall longevity of these teeth. In conclusion, orthodontic tooth movement can be performed on both healthy as well as diseased periodontium, provided physiologic orthodontic forces are used in conjunction with the control of periodontitis and meticulous oral hygiene throughout the treatment period .(Ong MA et al, 1998).
References
- Bollen A-M. Effects of malocclusions and orthodontics on periodontal health: Evidence from a systematic review. Journal of Dental Education 2008; Vol 72, No.8.
- Gkantidis N, Christou P, Topouzelis N.The orthodontic–periodontic interrelationship in integrated treatment challenges: a systematic review. Journal of Oral Rehabilitation 2010 37; 377–390
- Goldman HM,Cohen DW, PeriodontalTherapy, Mosby, St. Louis, Mo, USA, 1968.
- Kitaura H, Kimura K, Ishida M, Sugisawa H, Kohara H, Yoshimatsu M, Takano-Yamamoto T.Effect of cytokines on osteoclast formation and bone resorption during mechanical force loading of the periodontal membrane. Scientific World Journal. 2014.
- Laura Mitchell. An Introduction to Orthodontics. 4th Edition. 2013.Oxford University Press.
- Ong MA, Wang HL, Smith FN. Interrelationship between periodontics and adult orthodontics. J Clin Periodontol. 1998 Apr;25(4):271-7.
- Samah Alfuriji, Nora Alhazmi, Nasir Alhamlan,Ali Al-Ehaidep Moatzbellah, Nasser Alkatheeri and Amrita Geevarghese. The effect of orthodontic therapy on periodontal health: a review of the literature. Int J Dent. 2014.
- Zhi-Gui Ma, Chi Yang, Bing Fang, Yun Hui Xia,Li-Xia Mao, Yi-Miao Feng, Three-D imaging of dental alveolar bone change after fixed orthodontic treatment in patients with periodontitis. Int J Clin Exp Med 2015:8(2):2385-2391
| Last Reviewed | : | 28 August 2020 |
| Writer | : | Dr. Mah Eng Ching |
| Accreditor | : | Dr. Surguna Devi a/p Muniandy |
| Reviewer | : | Dr. Hjh. Rashidah bt. Dato’ Hj. Burhanudin |







