Personal Protective Equipment (PPE) protects healthcare workers from two main hazards, radiation and biological agents (virus, bacteria, etc). Biological agents transfer from person to person by direct or indirect contact. Health workers maintain close contact with patients. Thus, they need PPE that protects them from potential transmission. Important transmission pathways to mitigate with PPE include person to person contact, droplet spread, airborne transmission and contaminated objects (fomites).
According to WHO, the main characteristics of PPE include:
|
Category |
Characteristic |
|
Design feature |
1. Protect mucous membranes |
|
Material performance |
6. Able to protect for the duration of work period |
|
Use desirability |
9. Standardize donning and doffing protocol with minimum steps |
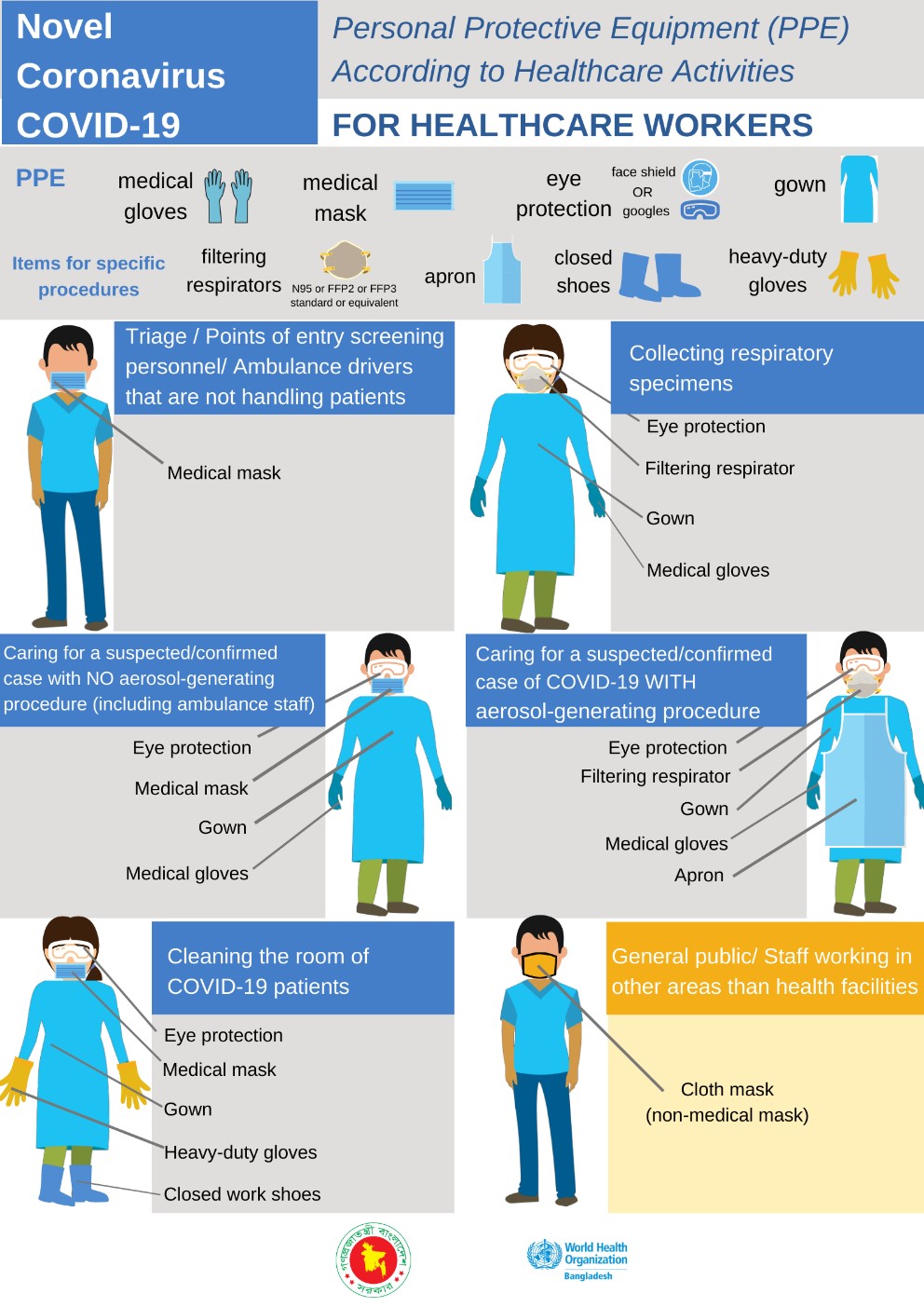
Below are examples of PPE commonly used in hospitals:
|
PPE |
Description |
|
Gloves |
Disposable gloves are worn by healthcare workers to protect their hands from contact with blood, body fluids, or contaminated surfaces. They can be made of latex, nitrile, or vinyl, depending on the individual’s allergies and the type of exposure anticipated. |
|
Masks |
Masks, such as N95 respirators or surgical masks, provide respiratory protection. N95 respirators filter out at least 95% of airborne particles, including small respiratory droplets containing infectious agents. Surgical masks protect against larger droplets but offer less filtration than N95 respirators. |
|
Face Shields & goggles |
These protect the eyes, nose, and mouth from splashes, sprays, and respiratory droplets. Face shields cover the entire face, while goggles protect the eyes specifically. |
|
Gowns |
Disposable gowns are used to shield the healthcare worker’s clothing and skin from contamination. They provide a barrier against contact with blood, body fluids, and other potentially infectious materials. |
|
Head covers & shoe covers |
Head covers (e.g., bouffant caps) and shoe covers are used to prevent contamination of the hair and shoes, respectively. |
Source: https://www.who.int/bangladesh/emergencies
PPE for Autopsy Cases
In autopsy cases, Personal Protective Equipment (PPE) is of utmost importance due to the potential exposure to infectious agents and hazardous materials during the examination of deceased individuals. Autopsy procedures involve the handling of body fluids, tissues, and organs, making it necessary for autopsy personnel to take appropriate precautions to protect themselves from potential health risks.
|
PPE |
Description |
|
Double gloves |
In autopsy procedures, wearing two layers of gloves is common. A primary pair of gloves made of latex, nitrile, or other suitable material is worn for examination, and a second pair made of a different material is worn over the first to provide an added layer of protection. |
|
Full-body coveralls or gowns |
Autopsy personnel typically wear full-body coveralls or impermeable gowns that provide complete coverage to protect against splashes and direct contact with body fluids and tissues. |
|
Face Shields & goggles |
Full-face shields or goggles are used to protect the eyes, nose, and mouth from splashes, blood, and other potentially infectious materials. |
|
Hair covers |
Autopsy personnel often wear bouffant caps or other hair covers to prevent hair from falling into the autopsy area and potentially becoming contaminated. |
|
Shoe covers |
Disposable shoe covers are worn to prevent the transfer of contaminants from the autopsy room to other areas. |
|
Respiratory protection |
Depending on the autopsy case and potential exposure risks, respiratory protection may be required. This can include N95 respirators or other appropriate respirators to protect against airborne infectious agents. |
|
Aprons or impervious sleeves |
Additional protection such as aprons or impervious sleeves may be used to cover specific areas, such as the forearms, during procedures. |

Source: https://doi.org/10.3389/fpsyg.2022.901244
Besides that, specialized biohazard bags and containers are required to safely collect and transport tissues, organs, and specimens for further analysis. Proper hand hygiene is essential before donning PPE, after removal, and any time there is potential contamination during the autopsy procedure. Handwashing with soap and water or using alcohol-based hand sanitizers is crucial.
It is important to follow established autopsy protocols and infection control guidelines when performing autopsies to minimize the risk of exposure to infectious agents. Autopsy personnel should receive training on proper PPE use, including how to don and doff PPE safely, and follow standard precautions to protect their health and well-being. Additionally, the use of engineering controls, such as adequate ventilation in autopsy rooms, can further enhance safety during autopsy procedures.
During autopsy cases involving infectious diseases or unknown pathogens, local health authorities and infection control experts may provide specific guidelines and recommendations for PPE use based on the nature of the case and potential exposure risks.
References
-
Changes to Ebola Protection worn by U.S Hospital workers
-
Jabatan Perubatan Forensik, Hospital Kuala Lumpur
-
https://www.who.int/teams/health-product-policy-and-standards/assistive-and-medical-technology/medical-devices/ppe
-
Loibner, M., Barach, P., Wolfgruber, S., Langner, C., Stangl, V., Rieger, J., … & Zatloukal, K. (2022). Resilience and protection of health care and research laboratory workers during the SARS-CoV-2 pandemic: analysis and case study from an Austrian high security laboratory. Frontiers in psychology, 13, 901244.
|
Last Reviewed |
: | February 2024 |
|
Writer / Reviewer |
: | Nurhusni binti Mohammad Room |







