Introduction
Early intervention programs supports the needs of the infants and toddlers with development delays and disabilities. Physiotherapist can helps the families with their child’s development and ability to participate in age-appropriate and meaningful activities. Physiotherapist provides therapeutic intervention to enhance the gross motor and fine motor development skills where they will work together with families, caregivers and other team members when necessary.
Early intervention should start early as possible so that it can improve the quality of the life of the children and reduce careers burden. Development delay describes the behaviour of young children whose development in moving, talking or playing is slower than other children of the same age. The delay can be in any areas of development such as movements, thinking, speech or self -care skills. Normally a child who is having development delay will have general lack of movement or does not move in a lot of different ways and even do not explore the movement.
Warning Signs Of Gross Motor Delay At Various Ages
| Normal Gross Motor Milestone |
Assessment Techniques |
Warning signs / Needs to refer to the doctor |
| Head control at 4-6 weeks |
Observe the : head control : elbow slightly Flexed
Source : www.beyondbasicplay.wordpress.com
|
Gross head lag by 6 weeks Observe for
Source: www.naturaltothecore.wordpress.com |
| Head control 6 weeks to <3 months |
:ability to lift chin off couch momentarily : bottom flat : forearm support
source : www.photo.elsoar.com |
Source : www. philnews.ph |
| Roll over at 3 months to 6 months |
Source : www.secretsofbabybehaviour.com Able to roll over
Source : www.pregnancyand baby.com |
|
| Sitting at 6 – 9 months |
source : www.zenbabyyoga.wordpress.com |
|
| Crawling at 8-10 month |
Source : www. photo.elsoar.com |
|
| Stand with support at 9 – 12 months |
WITH SUPPORT
Source : www.modernmom.com WITHOUT SUPPORT
Source www.getty.images.com |
|
| Walking at 12 – 15 months | Observe child’s walking ability | Unable to walk a few steps by 15 months. |
| Running at 18 – 24 months | Observe the child’s ability to run | Unable to run / run awkwardly by 24 months |
Handling and Position
An early handling techniques and correct position are very much important for a child with disabilities. This will enhance the child to move correctly from one place to another place. The correct handling and proper positioning is to provide a good body support and balance and ensuring safety of the child. Besides that, it also can avoid aggravation of abnormal tone and posture and minimize and prevent further deformity and injuries.
A correct handling and positioning skills are important to be carried out all the time once the abnormality of the child is detected. This is done when the child’s condition is stable. Because it will keep the child in a comfortable position all the time.
Parental involvement is crucial in the management of this child. Through training the mother/carer, it is possible to overcome the problems.
| Carrying / Lifting | Techniques | Explanation |
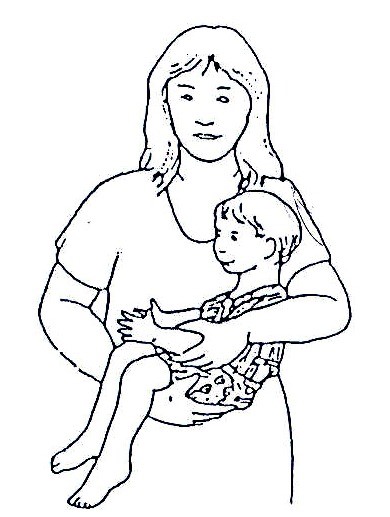
| Carrying a child |
Source : wikieducator.org/Lession _20_disability _and _rehabilitation_part_2. |
Carry him/her in a way which corrects abnormal positions and which brings both his/her arms forward. A more upright position helps him/her learn to hold his/her head up and look around. |
|
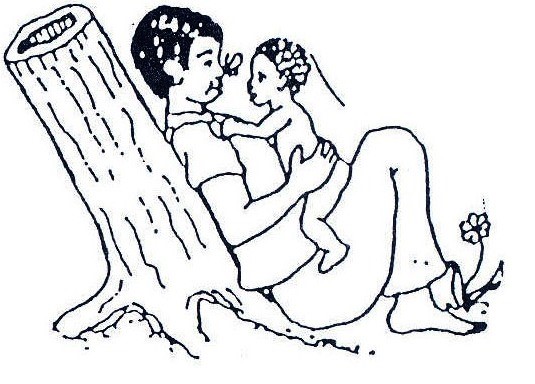
carrying a spastic child whose legs cross, or a floppy child |
Source : wikieducator.org/Lession _20_disability _and _rehabilitation_part_2. |
Facing the child face while playing with both legs apart. |
|
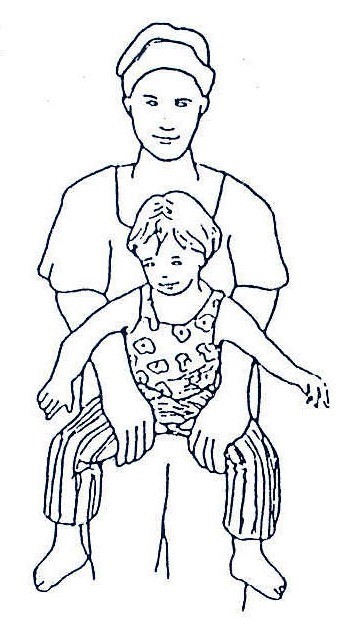
Carrying a spastic child. |
Source : wikieducator.org/Lession _20_disability _and _rehabilitation_part_2. |
Carry the spastic child or those having legs cross. You can swing him/her from side to side in this position. |
|
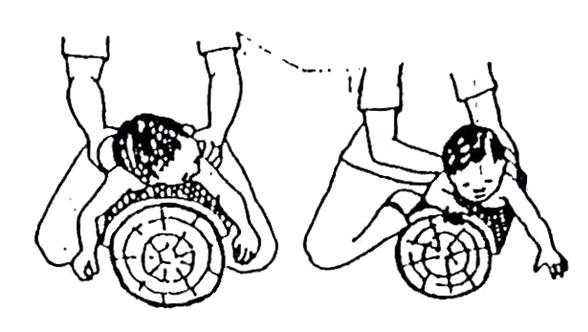
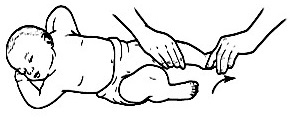
Position a child to a sitting position with facilitating head movements. |
Source : wikieducator.org/Lession _20_disability _and _rehabilitation_part_2. |
Play with him/her, supporting his body firmly but with his/her head and arms free. Attract his/her attention with interesting objects and sounds, so that he turns his/her head first to one side and then to the other. |
|
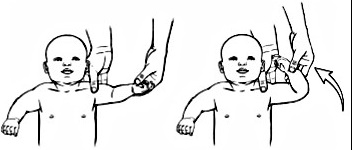
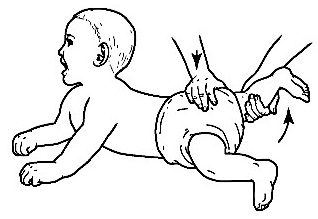
Positioning of neck, shoulder and arm |
Source: wikieducator.org/Lession _20_disability _and _rehabilitation_part_2. |
Position face down is a good position for a child to begin to develop control of the head, shoulders, arms and hands, and also to stretch muscles in the hips, knees, and shoulders. |
Range Of Motion Exercises
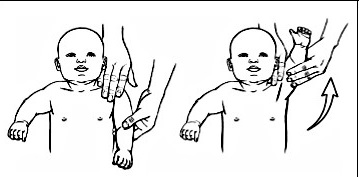 |
Raising arm above head Raise his arm so his hand is over his head with his thumb pointing up. Keep his elbow straight |
 |
Raising arm to side Move his arm to the side away from his body until it is straight out to his side. |
 |
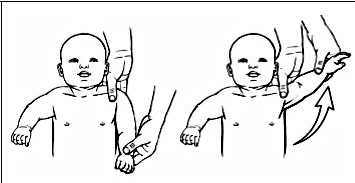
Move shoulder in circle Bent elbow at 90° angle and move shoulder in circle. |
 |
Bending elbow Bend his elbow and then straighten the elbow. |
 |
Rotate forearm up and down Turn his forearm and hand up and then down |
 |
Bending wrist. Move his hand forward and then move his hand back. |
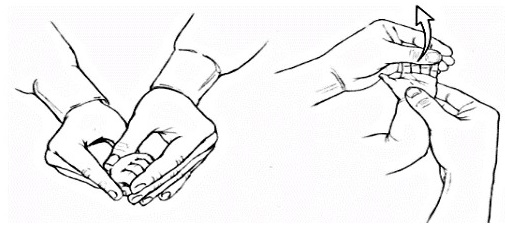 |
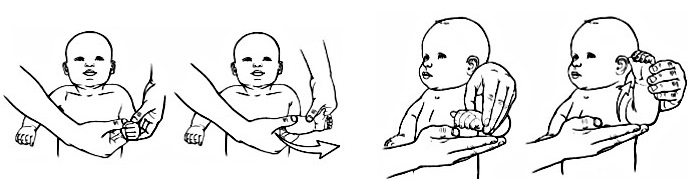
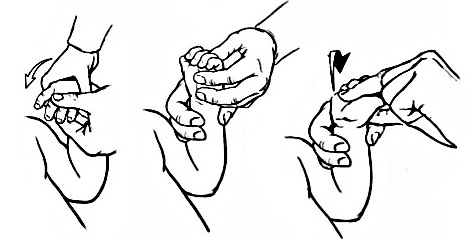
Closing and opening hand Bend his fingers and then straighten his fingers |
 |
Leg lift Lift the leg straight up while holding the hip and bottom in place. Gently hold for 3 seconds and take leg back down. |
 |
Bend and straighten hip and knee Bend the hip and knee up toward the belly and hold. (Figure B) Then straighten the leg down and hold ( Figure A) |
 |
Bend foot down Bend the foot down and hold for 3 seconds. Then return to the starting position. |
Source : Leg Range of Motion – baby (Wexner Medical Center) : Exercises Upper Extremities infant (Nationwide Children’s Hospital)
Important points to remember when carrying-out the range of motion exercises
- Do the exercises very gently. Closely watch the infant’s face for signs of pain or discomfort.
- Do each motion 10 to 15 times and NOT to the end of the range of motion. Move into the range until mild resistance is felt and hold there for 30 seconds. Do not bounce into this stretch.
- Do one joint at one time.
- Never Force the movements. Range of motion exercises may cause some discomfort but should NOT be painful.
Conclusion
Development delays should be identify and treated as early as possible, as children’s brains can change easily and also can respond to training that will help them learn the skills that are lacking. Co-operation from parents and therapist is needed to determine full success.
References
- Family health Development Division Ministry Of Health Malaysia, 2001, Manual on the management of children with gross motor delay.
- www.drnathbrachialplexes.com
- www.specialeducationalneeds.co.uk/global-developmental-delay.
| Last Reviewed | : | 23 August 2019 |
| Writer/Translator | : | Kogilavani a/p S.Krishnan |
| Accreditor | : | Se To Phui Lin |
| Reviewer | : | Halimah bt. Hashim |