Definition
Burns are injuries to the skin caused by material which are exposed to heat, chemicals, friction, ice, electric shock or radiation.
Injury classification:
a) Injury of burns are divided into: –
1. Heat (thermal injury) – fire, flammable liquids such as gasoline, gas, hot water, hot steam.
2. Chemical injury – acid etc
3. Electrical injury – electrocution, lightning.
4. Radiation injury – solar energy, radiotherapy and laser
5. Ice burn – frost bite
b) Total Body Surface Area Burns (Percentage)
i) Rule of Nine
iii) LUND-Browder Chart
iii) Palm’s Rule
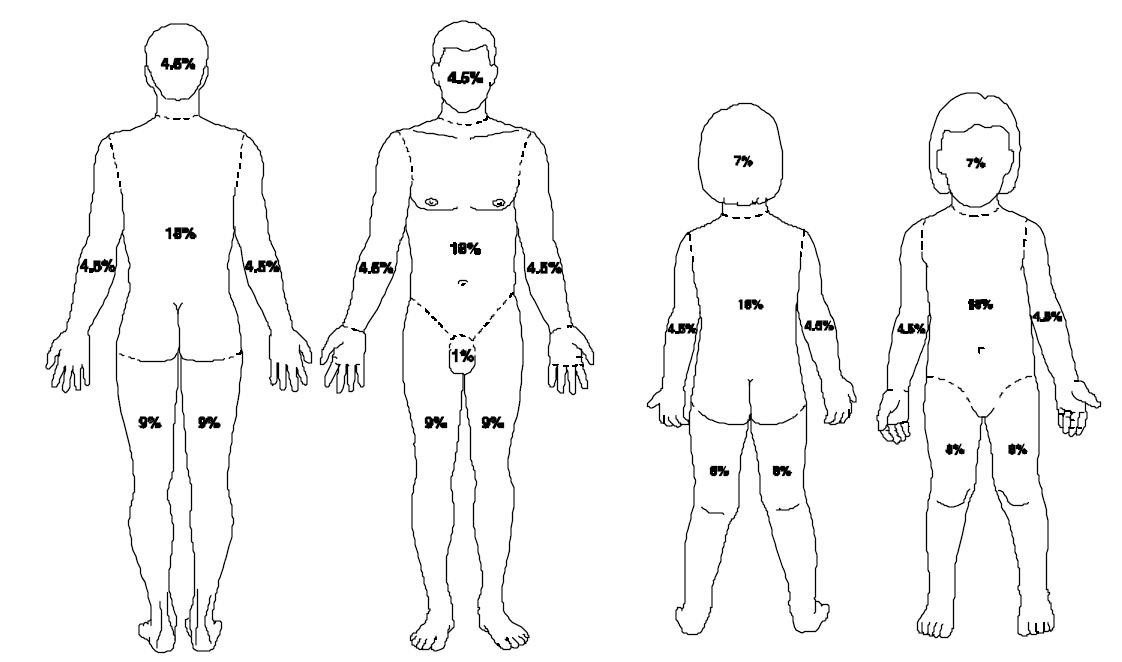
Figure: Rule of Nine
c) Degree of Burns
|
Degree of Burns |
1st degree |
2nd degree |
3rd degree
|
4th degree |
|
|
Superficial |
Deep |
||||
|
Layer of skin involved
|
Epidermis – the outer layer
|
Dermis-outer layer
|
Dermis-inside layer
|
Subcutaneous fat
|
Involve the muscles, tendons, and bones
|
|
Sign and Symptom |
Redness, pain
|
Pink / red, blister, moist, sore
|
Dry, white and non blanching |
Leathery, dry, white or red with thrombosed vessel |
Black ,charred with eschar dry |
|
Healing time |
3-7 days |
10-14 days |
17- 21 days, require skin graft
|
Require skin graft |
Require reconstruction |
d) Inhalation Injury
Inhalation injuries refer to respiratory tract injury caused by inhalation such as smoke inhalation
Inhalation injuries are divided into 3 types:
i. upper respiratory tract (larynx and vocal cord)
ii. the main airways (tracheobronchial tree)
iii. terminal airways (bronchioles and alveoli)
|
Level |
Duration |
Physiology |
|
1st Level |
3 to 8 hours |
Difficulty breathing (respiratory distress) is minimal as a result of bronchospasm or damage to the alveoli or both |
|
2nd Level |
8 to 48 hours |
Obstruction of the respiratory tract caused by edema of the upper respiratory tract or lower or both. |
|
3rd Level |
After 72 hours |
Pneumonia, often caused by gram-negative organisms |
Inhalation Injury Complications
1. Tracheal Stenosis
2. Trachea Inflammation
3. Tracheal Ulcers
4. Granuloma Formation
Physiotherapy Management
Treatment of burns cases can be divided into 3 phases: –
- Acute Phase (Acute)
- Sub-acute phase (Subacute)
- Healing and scar maturation Phase (Post Epithelial healing)
Acute phase:
1. Respiratory Care, help to maintain or regain optimal respiratory function. Respiratory care is very important especially for cases of inhalation injury and burns to the chest. Chest physiotherapy is very important and the techniques are: ·
- Breathing exercises
- ACBT (active cycle of breathing technique)
- Manual techniques of chest physiotherapy – Percussion, Vibration
- Postural drainage or Modified Postural Drainage
- Suction (if necessary)
- Thoracic mobility exercises
- Positioning
- Adjunct: Incentive spirometer, flutter if necessary
2. Positioning to the joint Involved
The correct position is at odds with the comfortable position and contractures. Performed on the first day of the patients admitted to hospital until the scars mature. Joint involved are positioned correctly to achieve goals such as: –
- Reduce swelling
- Prevent deep vein thrombosis
- Prevent further damage to the joints or exposed tendons
- Avoid damage to new skin graft.
- Avoiding pressure sores occur in certain area – such as the styloid process, the medial malleolus, the lateral malleolus and the Achilles tendon.
- Maintain range of motion to prevent contractures Positioning Techniques:
|
Burns Area |
Deformity |
Position to prevent contracture |
Technique |
|
Head/Neck
|
Flexion |
Extension or slight hyperextension |
Roll the towel and placed below the neck. |
|
Elbow
|
Flexion
|
Extension and Supination |
Use Arm troughs, pillows or splints
|
|
Wrist and fingers |
Flexion
|
Extension Of wrist and fingers |
Put Arm troughs, pillows or splints
|
|
Hip
|
Flexion, External rotation |
Hip Extension and lower limb in neutral position. |
Lying supine or prone positions. No pillow under the knees.
|
|
Knee
|
Flexion |
Extension
|
No pillow under the knees. |
|
Ankle
|
Plantar Flexion |
90 degree dorsi flexion. |
Pillow or splint to support the ankle. |
Notes :The correct position should always be continued until maturity to avoid scar contractures.
3. Therapeutic Exercise
Exercise should be done on the first day of admission until the scars mature. The purpose is to:
- Maintain Joint integrity
- Maintain muscle flexibility and elasticity of the skin
- Maintain range of motion to prevent contractures
- Increase muscle strength and endurance.
- Restore the musculoskeletal function to optimal level.
Soaked During Exercise
- The ideal time to exercise is when soaked in warm water to soften the tissue and provide comfort to patient.
Sub-acute phase
1.Continue with respiratory care
2.Continue with therapeutic exercise
3.Continue with the joint involved in the correct position
4.Do mobility movement / ambulation
Ambulation
Ambulation will start once:
- Haemodynamic status is stable
- There are no signs of active bleeding in the joint involved
- Bandaging of affected area is done
Action should be taken if there are signs like the following:
|
Signs |
Action |
| Increase of oedema |
Elevate the limb involved |
| Damage to the healed skin |
Refer to the doctor in-charge |
|
Increase of pain |
Pain management / Refer to the doctor in-charge |
Precautions:
- The movement of the hip joint cannot be moved if there are Femoral Intra Venous inserted unstable vital signs
Healing and scar maturation phase (Post Epithelial Healing)
- Therapeutic exercise for circuit training so that patients are more independent.
- Stretching exercises
- Muscles strengthening exercise such as using Theraband, weights, dumbbells, etc
- Exercise to increase endurance. Examples of aerobic exercise such as climbing stairs.
- Exercise to improve coordination such as Proprioceptive Neuromuscular facilitation (PNF)
- Home exercise
- Do exercise continuously until scars are matured
- Elevation of the joints involved if there is swelling,
- Encourage to do activities of daily living.
Scar Care
Scarring of burn wound is a continuous process. Scar will stop when the skin is ripe. Understanding patient’s care related to scarring should be intensified to prevent the growth of hypertrophic scar Clinical presentations of a matured scar:
- Soft
- Align
- No tension in the scar
- Scars return to original skin tone
Hypertrophic scar have clinical features as below: –
- Redness of surface
- Surface scars arising
- Less flexibility
- Pain and itch
 |
 |
Scar management:
a. Scar massage
The manipulation of soft tissue combined with stretching can reduce scar formation. The manipulation of scars:-
- Encourage the restoration of collagen
- Helps to reduce irritation
- Maintains moisture and elasticity
Scars Massage Technique: –
- Apply the lotion on the affected area. Use unscented lotion.
- Apply pressure to the skin sufficiently
- 3-way massage which is rounded up and down, and side to side
- Sort through friction techniques more effective if combined with stretching and exercise.
- Perform 3-4 times per day.
Skin care
i. Hygiene
- Test the water temperature before entering the tub or shower because the new skin more sensitive to the water temperature.
- Clean out by using a plain water to shower.
- Use a soft, clean towel to wipe
ii. Dry skin
The skin looks dry and scaly as a result of the destruction of oil refineries.
- Use lotion or moisturizer to keep the skin moist.
- Stay away from oils containing lanolin and alcohol resulting blister burns / blisters on the skin that is new.
iii. Sun light
New heal skin is more easily injured when exposed to sunlight – ultraviolet rays.
- Wear long-sleeved dress, trousers, big hats to protect the wound. Do activities in the early morning or late afternoon.
- Avoid exposure to direct sunlight. Apply cream / lotion to prevent ultraviolet ray
iv. Cold weather
Patients will experience a spectrum of sensory numbness in the tips of the toes and hands.
- Wear thick clothing and stay away from exposure to cold weather too long.
v. Itchy skin
Dry skin will cause the patient to experience irritation.
- Wear loose clothing to avoid sweating• Avoid scratching the heal skin because it is very thin, sensitive and easily hurt
- Use lotion intensively.
vi. Burns / blisters
The new skin is easy to burn / blister caused by pressure and friction.
- Avoid wearing clothes or shoes that are too tight.
General Prevention:
Hand Washing:
1. Dry hands according to proper procedure
2. Hands should be washed: –
- Before and after treating / touching patients
- After handling objects that are exposed to the fluid and the patient
References
- Burns and scalds , Clinical Knowledge summaries ( 2007 )
- Edger .D (2004 ) Rehabilitation after Burn Injury, BMJ 2004, 343-345
- Enoch S, Roshan A, ShahM: Emegency and early management of burns and scalds.
- Garis Panduan Perawatan Kes Kelecuran, Jawatankuasa Teknikal Profesion Fisioterapi, Bahagian Sains Kesihatan Bersekutu, Kementerian Kesihatan Malaysia.
- M.M, Cox.K Crawford .C. Werth.D (1987) .Burn Care and Rehabilitation Gene and Barbara Burnett Burn Centre kansas University Medical Centre Kansan City, kansas U.S.A
- Co.Uk- trusted medical information and support. http://www.Patient.co .uk/doctor/burns -Assessment-and-management.htm (accesed) 17 /5/2012.
- Physical Therapy Journal of the American Physical Therapy Association
- Ronald P. Mlcak a, Oscar E. Suman, David N. Herndon (2007), Respiratory management of inhalation injury.
- Standard of care: Inpatient Physical management of patients with Burns. Brigham and Women’s Hospital (2008)
- myhealth.gov.my/.cara-membasuh-tangan-yang-betul
| Last Reviewed | : | 23 August 2019 |
| Writer | : | Pauzilah binti Hj Dollah |
| Translator | : | Sahira Nadiah Shirlen binti Oyon |
| Accreditor / Reviewer | : | Halimah binti Hashim |


















