Introduction
Pre-implantation genetic diagnosis or PGD is a genetic testing that has been performed on gene and chromosome of the embryo produced through in vitro fertilisation (IVF) technique to detect specific genetic diseases and chromosomal disorders. PGD is a technique that aimed to screened couples at risk, and enable them to avoid inheritable disease to their children.
Chromosomes is made out of protein and a single molecule of deoxyribonuclei acid (DNA) that passed from parents to offspring. This carry the gene that contain the genetic material to define the individual and also provide the instructions that tell the embryo how to develop into a baby. Each cells should have exactly 46 chromosomes where sperm and oocyte each have 23 chromosomes. If chromosomes are lost or been duplicate, the genetic instructions no longer make sense and the embryo will be unable to form a healthy baby.
History
First known biopsy on embryo was perform by Edward and Gardner on rabbit embryos in 1968. As an alternative to current prenatal diagnose, PGD has been developed in the United Kingdom for human since 1980s. Initially this technique has been revolved to determine the gender of embryo as an indirect means to avoid an X-linked disorder. Currently, PGD is available for most genetic mutation like trisomy 18 (Edward syndrome), trisomy 21 (Down syndrome), and X,Y-linked disease.
Importance
PGD enable couples at risk of passing on an inherited disorder to significantly decrease the risk of having an affected child. This technique is also one of the option for couples to become a parent without risking the need for termination of pregnancy.
PGD is for:
- Those who already have child with serious genetic condition
- Those who ended their previous pregnancy because of serious genetic disease (termination of pregnancy)
- Those with a family history of serious genetic disease
- Those with a family history of chromosome problem
Procedure
PGD is a technique that involves testing cell(s) from embryos created outside the body by IVF for a genetic disorder. Tests are carried out for the specific disorder that the embryo are known to be at significant risk of inheriting. Unaffected embryo will be selected for transfer to the uterus in hope that a normal birth will ensue.PGD is completed with IVF/ICSI-(intracytoplasmic sperm injection) started from ovarian stimulation, egg recovery, fertilisation, embryo biopsy, genetic testing and single fresh embryo transfer.
Removal of the PB, and cells from the embryo requires access to perivitelline space of the oocyte through an opening of the zona pellucida. There are three different method in principle for opening the zona; through acidic tyrode solution, mechanical, or laser dissection.
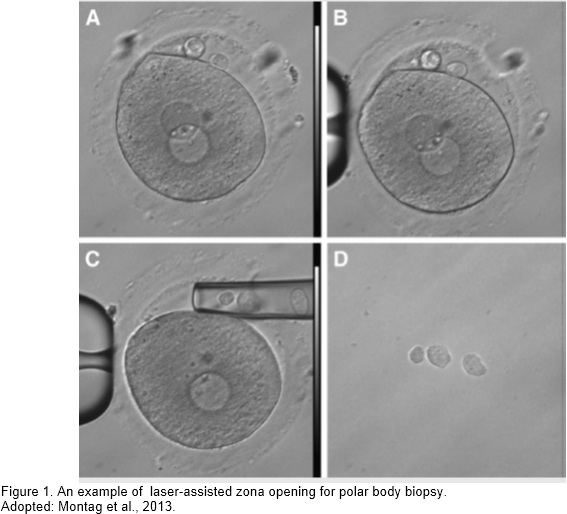
- Positioning the oocytes with both polar bodies aligned in one focal plane
- A precised opening of the zona is introduced by 2-3 laser shots
- A blunt biopsy cappilary are introduced to aspirate the polar bodies
- Released of the polar body in a spearate droplet in the same dish for further process.
- Stages or timing of embryo biopsied
Biopsied will be performed on oocyte or cell(s) from embryo before any screening was done to detect their genetic problem. There are three different timing of biopsy:
- Polar body (PB) biopsied that involved the first, second or both polar body

This type of biopsy was performed on egg or oocyte at the early stage of the egg. Known as a non-invasive technique, this biopsy could obtain an early specimen and allow more time for laboratory analysis and fresh transfer in IVF patients to be perform. Two ways of performing PB biopsy, either with first PB biopsy before insemination process were done, subsequentially followed with second PB biopsy after fertilisation or both PB are biopsied after the fertilisation process and screened altogether. This stage of biopsy have been performed to obtained female or maternal part of an error without disturbing the developing embryos (Brezina et al., 2013).
- Blastomere biopsy or cleavage stage embryo that usually perform on day 3 embryo
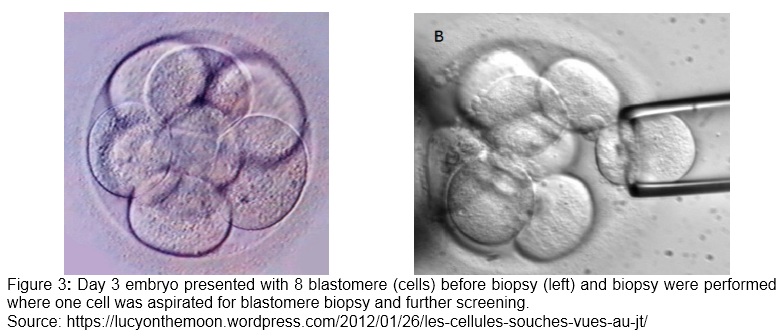
Biopsy on one or two cells (blastomere) of embryo during cleavage stage (Figure 3) for PGD in detecting paternally originated or post meiotic aneuploidy that occur after fertilisation and able to perform fresh embryo transfer prior to the analysis.
- Blastocyst or trophectoderm biopsy on day 5 embryo

In contrast with single cells biopsy during blastomere stages, trophectoderm biopsy are possible to screen multiple cells, which means that number of copies DNA are increased and better screening of aneuploid with PGD are possible (Scott et al., 2013). Due to timing of biopsy that are performed on day 5 onwards, and the results of screening are only available within 24 hours post biopsied, fresh transfer for this embryo biopsied are not possible. Thus, it is important to have a good cryopreservation program in order to feasible the blastocyst biopsy and minimal loss of the euploid embryo (Adler et al, 2014)
- Polar body (PB) biopsied that involved the first, second or both polar body
- Methods of genetic screening
PB or cells biopsied from either blastomere or trophectoderm biopsied were analysed for their genetic material screening known genetic diseases. The type of technologies in identifying some or all chromosome pairs up to individual chromosomes and its parental origin for aneuploidy testing in IVF patients are also important. Whether the technologies are time consuming, cost-effective, in-house clinical set up or outsource to a service lab, this technologies need to balance between the benefits of identifying euploid embryo with the potential costs to the embryo involving those invasive biopsies and any false positive or negative test results (Handyside 2013).
The first molecular cytogenetic technique in aneuploidy testing was; fluorescence in situ hybridization (FISH) with a combination of chromosome-specific probes labeled with different fluorochromes. However, this technology are only efficient in screening approximately from 12 to 14 chromosomes which suite for PGD that screen a know location of chromosomal error such as trisomy 21, X- and Y-linked chromosomes.
Polymerase chain reaction (PCR) is used for the diagnosis of single gene defects, including dominant and recessive disorders. Where a particular DNA sequence is copied many times in order to facilitate its analysis. PCR provides the possibility to obtain a large quantity of copies of a particular genome for further analysis. Although the technique is highly sensitive and specific, a sufficient amounts of a pure, high-quality sample of DNA, which is sometimes difficult to obtain from a single cell.
In addition, single cell genome sequencing is a new technique develop to sequence the whole complete DNA of the embryo. Through developing next generation sequencing, PGD is performed using targeted strategy and multiplex PCR reaction that include both the mutation site and the chromosome specific target sequence required. This technology has reduced the necessary of read depth for accurate sequencing of the mutation site, which reduces the time required and cost.
Risk and Considerations
Other than the important of timing of the biopsy, and the methods that have been used for screening in PGD, there are also other factors that need to be considered in performing PGD for patients that undergo IVF treatment. Such as the presence of mosaicism in those developing stage of embryo through blastomere biopsy (Brezina et al., 2013, Scott et al., 2013a). This is a condition where; in a single developing embryo, euploid (normal) and aneuploid cell lines are present and this condition might produce a result that is not representative of the entire embryo (Brezina et al., 2013).
With this phenomenon, rise another question whether genomic sequence of those single or two cells biopsied are enough to represent the whole entire embryo? During ESHRE PGD consortium in 2011, it was well documented about the disadvantage of performing biopsy on the blastomere stage of embryo include negative impact on clinical outcome by more than single cell biopsied and low survival rate of cryopreserved blastomeres embryo compared with blastocyst stage embryo (Harton et al., 2011).
Other than that, the ‘self correct’ theory in embryo, seems to be a technical challenges to perform PGD and the important of results interpretation to avoid misdiagnosis or false-positive results. In some cases, evidence suggest that embryo biopsy actually may ‘correct’ abnormality (Magli et al., 2000, Munné et al., 2005) which embryo mosaicism must no be considered abnormal before reanalyzed during blastocyst stages and discarded for abnormalities (ASRM, 2008). Although other factors such as the accuracy of method of screening used in those research related to ‘self-correct’ in aneuploid embryo could be questioned, however, their observation of those findings acknowledge that PGD results related to time of biopsy performed could be miss interpreted.
Regardless the biological factor involved and how accurate the advance technology in determining the results of aneuploidy screening in potential embryo, performing the biopsy itself, could be challenging as embryo or eggs should be treated with tender and cautions. Those embryos are precious and ‘contain’ such hopes of success from the couple that undergo IVF treatment.
There are evidence that performing biopsy on embryo could give adverse effect during zona breaching performed with acidic Tyrodes and laser (Montag et al., 2004, Harton et al, 2011). Even zona breaching could give adverse effect toward embryo biopsy, reconsidering reanalysis of possible ‘self correct’ed embryo or ‘unable to diagnose’ embryo, is it going to give more benefits rather than stress and trauma toward the embryo? This also could be related to the important of experienced, proficient and fully trained technician or embryologist to perform embryo or egg biopsy as suggested by EHSRE group for interest in PGD consortium in 2011 (Harton et al., 2011).
Couples at risk with genetic inherited disease to their offspring should also considered all the risk involved during IVF treatment such as ovarian hyper stimulation syndrome (OHSS), risk of mutiple pregnancies and risk of having an affected child. Nevertheless, prenatal diagnosis is still available for women conceive following PGD.
Outcomes
PB biopsy might be the optimal time to perform biopsy and determining 40 % aneuploidy screening from nondisjunction in meiosis I (Scott et al., 2013a). In some country such as German that came out with embryo protection act on illegal use of embryos “for any other purpose not serving its preservation”, PB biopsy would be the best timing for PGS. However, German’s researcher have contradicted with the law of German’s legal restriction, where they reported aneuploidy testing on PB of oocyte may not improve reproductive outcome (Haaf et al., 2010).
Although there are pro and cons in performing oocyte or embryo biopsied for PGD, this genetic screening method has been reported to reduced embryo loss after implantation through aneuploidy detection and able to improve live birth rates compared with natural conception in couples with recurrent miscarriage carrying a structral chromosome abnormality (Franssen et al., 2010).
References
- Adler A., Lee H.L., McCulloh D.H., Ampeloquio E., Clarke Williams M., Wertz B.H., & Grifo J. Blastocyst culture selects for euploid embryos: comparison of blastomere and trophectoderm biopsies. Reprod Biomed Online. 2014;28 (4):48591
- Brezina P.R., Kee R.W., & Kutteh W.H. Preimplantation Genetic Screening: A Practical Guide.
- Clinical Medicine Insights: Reproductive Health. 2013;7:37-42.
- Haaf T., Tresch A., Lambrecht A., Grossmann B., Schwaab E., Khanaga O., Hahn T., & Schorsch M. Outcome of intracytoplasmic sperm injection with and without polar body diagnosis of oocytes. Fertil Steril. 2010;93 (2):40515.
- Handyside A.H. 24-chromosome copy number analysis: a comparison of available technologies. Fertil Steril. 2013;100 (3):595602.
- Harton G.L., Magli M.C., Lundin K., Montag M., Lemmen J., Harper J.C., European Society for Human Reproduction and Embryology (ESHRE) PGD Consortium/Embryology Special Interest Group. Best practice guidelines for polar body and embryo biopsy for pre implantation genetic diagnosis/screening (PGD/PGS). Hum Reprod. 2011;26 (1):416.
- Magli M.C., Jones G.M., Gras L., Gianaroli L., Korman I., & Trounson A.O.. Chromosome
- Scott, R.T, Upham, K.M., Forman, E.J., Hong, K.H., Scott, K.L., Taylor, D., Tao, X., & Treff, N. R. Blastocyst biopsy with comprehensive chromosome screening and fresh embryo transfer significantly increases in vitro fertilization implantation and delivery rates: a randomized controlled trial. Fertil Steril. 2013;100 (3):697703.
| Last Reviewed | : | 14 April 2016 |
| Writer | : | Siti Norfaizah bt. Wagiman |
| Accreditor | : | Krishnan a/l Kanniah |







