Psoriatic arthritis (PsA) is an inflammatory joint disease associated with psoriasis which is a skin disease. PsA affects women and men equally. PsA may occur in up to 30% of patients with psoriasis. Among Malaysian patients with psoriasis, approximately 15-20% have PsA. The arthritis appears after the onset of skin lesions in the majority of patients with PsA. However, the arthritis may precede the skin disease in approximately 13-17% of patients. Undiagnosed arthritis in the presence of skin lesions represents an additional 15%. The extent of skin disease does not generally correlate with the severity of joint disease.
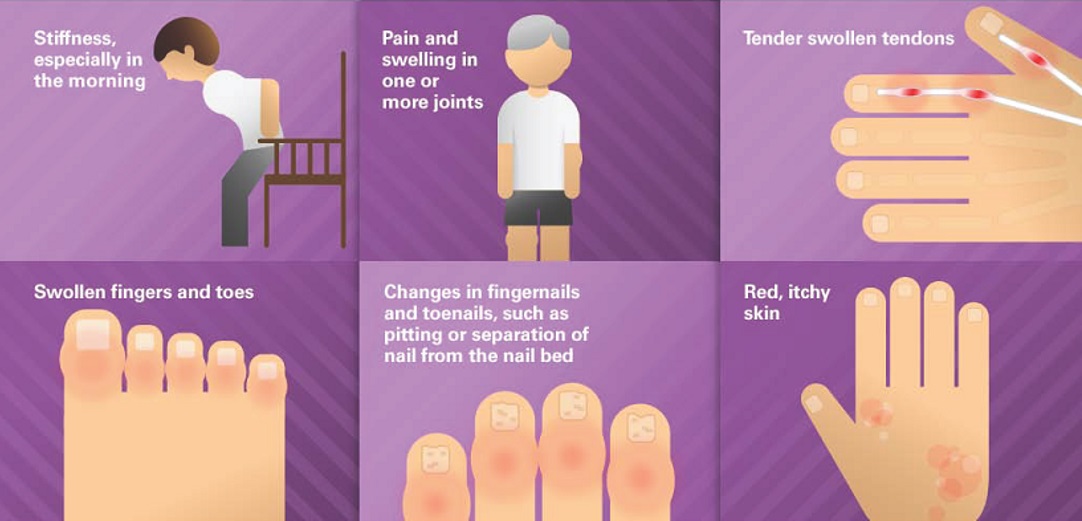
Signs and Symptoms
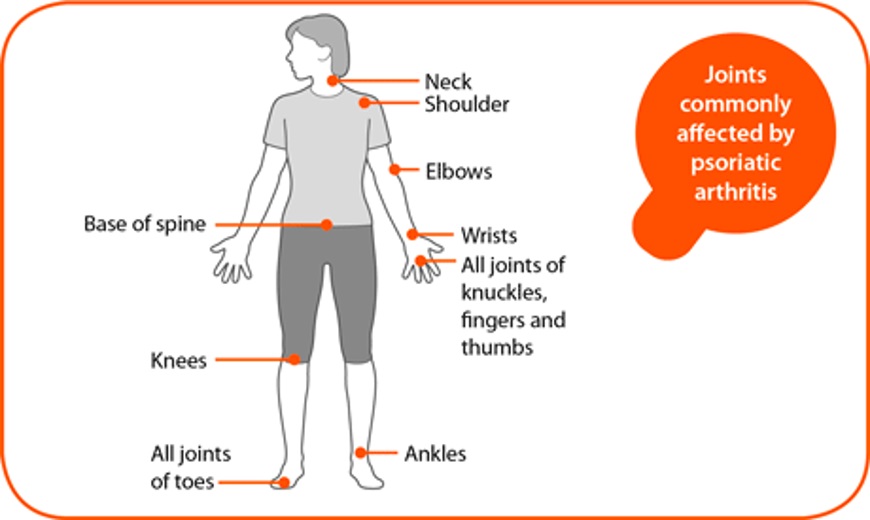
PsA may present in a variety of joint manifestations. PsA may involve peripheral or limb joints, axial or spinal joints, or both. It frequently presents as polyarthritis (many joint involvement) or less often as oligoarthritis (few joint involvement). Additionally, enthesitis (inflammation at the site of the insertion of tendons, ligaments, and synovium into bone), tenosynovitis (inflammation of the protective sheath around tendons), and dactylitis (swelling of an entire finger or toe, termed a “sausage digit”) may also occur.
 |
| Source: www.liberatehealth.us/liberate_condition/psoriatic-arthritis-2/psoriatic arthritis/ |
Patients with PsA present with pain and stiffness in the affected joints. The joint stiffness is usually worse in the morning and lasts more than 30 minutes. The stiffness is accentuated with prolonged immobility and is alleviated by physical activity. About 70% of patients presenting with arthritis will give a positive history of psoriasis. On physical examination, pain and swelling of the affected joints can be appreciated.
Clinical Patterns of Psoriatic Arthritis
There are five distinct patterns of PsA:
- Distal arthritis, characterized by involvement of the distal interphalangeal joints
- Asymmetric oligoarthritis, in which less than five small and/or large joints are affected in an asymmetric (unequal) distribution
- Symmetric polyarthritis, similar to Rheumatoid Arthritis
- Arthritis mutilans, characterized by deforming and destructive arthritis
- Spondyloarthritis, including both sacroiliitis and spondylitis
These patterns can often overlap.
 |
| Source: http://www.arthritisresearchuk.org/arthritis-information/conditions/psoriatic-arthritis/symptoms.aspx |
Investigation
Laboratory findings in PsA are non-specific, reflecting only the typical responses seen in acute as well as chronic inflammation. There are no laboratory findings that are characteristic of PsA, and none to distinguish it from other forms of inflammatory arthritis. However, investigations such as imaging and joint fluid analysis may be performed to exclude other joint diseases including rheumatoid arthritis, osteoarthritis, gout and reactive arthritis.
Treatment
The aim of treating PsA is to control inflammation and to prevent discomfort and damage to the joints. Whenever possible, the treatment should be coordinated between the rheumatologist and the dermatologist since there are differences in response between skin and joints with some agents.
The treatment strategy for PsA should begin with an assessment of the degree of disease activity and damage; referral of all patients for physical and occupational therapy, including exercise instruction, joint protection, and appropriate orthotics; education regarding the disease and the effects of stress on the illness; and instruction in the proper use of topical and oral medications.
Non-steroidal anti-inflammatory drugs (NSAIDs) alone are sufficient for mild disease, but a non-biologic disease-modifying anti-rheumatic drug (DMARD) like methotrexate (MTX) is preferred if the arthritis remains active despite NSAIDs5. Leflunomide or sulfasalazine may be used as alternatives to MTX.
 |
| Source: Department of Dermatology, Hospital Kuala Lumpur |
In patients with joints involvement not improving after treatment with MTX, a treatment with biologics should be considered. The biologics available for PsA treatment include Adalimumab, certolizumab pegol, golimumab (tumor necrosis factor (TNF) inhibitor), Ustekinumab (interleukin(IL) -12/23 inhibitor), secukinumab (interleukin(IL) -17 inhibitor). Use of oral glucocorticoids in patients with PsA should be avoided, except in acute flares of arthritis.
 |
| Source: Open access, Google Images |
How to prevent deformity
Early recognition and early initiation of treatment is key to preventing joint destruction and subsequent loss of function. This can be achieved with a multidisciplinary strategy of treatment that includes the rheumatologist, dermatologist, physical and occupational therapist, combined with intensive patient education regarding the disease and adherence to treatment.
Reference
- Malaysian Psoriasis Registry Annual Reports 2007-2011
- Wright V, Moll JM. Psoriatic arthritis. Bull Rheum Dis 1971; 21:627
- Cohen MR, Reda DJ, Clegg DO. Baseline relationships between psoriasis and psoriatic arthritis: analysis of 221 patients with active psoriatic arthritis. Department of Veterans Affairs Cooperative Study Group on Seronegative Spondyloarthropathies. J Rheumatol 1999; 26:1752
- Cuéllar ML, Citera G, Espinoza LR. Treatment of psoriatic arthritis. Baillieres Clin Rheumatol 1994; 8:483
- Chandran V, Schentag CT, Gladman DD. Reappraisal of the effectiveness of methotrexate in psoriatic arthritis: results from a longitudinal observational cohort. J Rheumatol 2008; 35:469
- Heiberg MS, Kaufmann C, Rødevand E, et al. The comparative effectiveness of anti-TNF therapy and methotrexate in patients with psoriatic arthritis: 6 month results from a longitudinal, observational, multicentre study. Ann Rheum Dis 2007; 66:1038
- Saad AA, Symmons DP, Noyce PR, Ashcroft DM. Risks and benefits of tumor necrosis factor-alpha inhibitors in the management of psoriatic arthritis: systematic review and metaanalysis of randomized controlled trials. J Rheumatol 2008; 35:883
- Gottlieb A, Menter A, Mendelsohn A, et al. Ustekinumab, a human interleukin 12/23 monoclonal antibody, for psoriatic arthritis: randomised, double-blind, placebo-controlled, crossover trial. Lancet 2009; 373:633
| Last Reviewed | : | 23 August 2019 |
| Writer | : | Dr. Rajalingam a/l Ramalingam |
| Accreditor | : | Datin Dr. Asmah bt. Johar |
| Reviewer | : | Dr. Nazatul Shima bt. Abd Rahim |







