Introduction
Pulmonary vascular diseases are a group of disease that affect the blood vessels along the route between the heart and lungs
Causes
- Pulmonary embolism
A pulmonary embolism happens when the blood flow through the lung’s artery is blocked suddenly. This is caused by a blood clot that has dislodged and traveled from somewhere else in the body usually the vessels from thelegs. A blood clot that forms in a vein of the leg, breaks free, travels through the heart and lodges in the lungs (thromboembolism). Large pulmonary emboli are fatal, causing sudden death.A number of other substances can travel through the blood stream to the lungs but they are much more rare: large bubble of air, ball of fat from fractured long bones or amniotic fluid during or after child delivery.
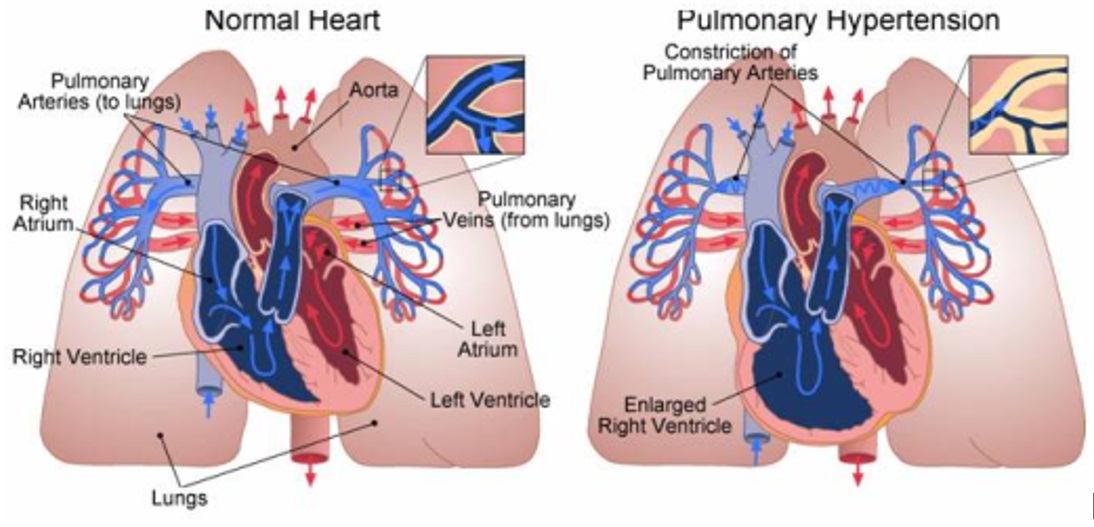
- Pulmonary hypertension
This is a disease that causes stress on the heart when the blood pressure in a person’s pulmonary arteries gets dangerously high. It affects the arteries in the lungs and the right side of your heart. Pulmonary hypertension begins when tiny arteries in your lungs, called pulmonary arteries, and capillaries become narrowed, blocked or destroyed. This makes it harder for blood to flow through your lungs, and raises pressure within your lungs’ arteries. As the pressure builds, your heart’s lower right chamber (right ventricle) must work harder to pump blood through your lungs, eventually causing your heart muscle to weaken and eventually fail. Pulmonary hypertension can be due to the effects of other diseases involving the heart, lungs, chronic thromboembolic disease and others. This can lead to strain on the right side of the heart, a condition known as cor pulmonale. When there is no apparent cause, it’s called idiopathic pulmonary arterial hypertension.
- Pulmonary edema
Pulmonary edema is a condition where there is a leakage of fluid from capillaries of the lung into the alveoli (or air spaces). It is usually caused by heart failure, with a rise in the vein’s blood pressure going through the lungs. As the pressure in the blood vessels increases, fluid is pushed into the lungs and causes a shortness of breath.Pulmonary edema may be caused by kidney failure, liver failure, exercise at very high altitudes (high altitude pulmonary edema), direct damage to the lung (by poisonous gas or severe infection), as a side effect of medications, or from major trauma. Pulmonary edema may also be a complication of any heart disease that causes the heart muscle to weaken or heart valves become stiff or damage.
- Pulmonary hemorrhage or bleeding into the lungs
Pulmonary hemorrhage is due to inflammation and damage to capillaries in the lung resulting in blood leaking into the alveoli. This can be either slow, long-term bleeding or it can be sudden and very serious. It may also be localised to one part of the lungs, known as the focal pulmonary haemorrhage or the bleeding can occur throughout the lungs, diffuse pulmonary haemorrhage may result in blood to be coughed up.Causes of focal pulmonary haemorrhage:
- Chest infection or pneumonia
- Tuberculosis
- Lung cancer
- Bronchiectasis
- Lung abscess
- Fungal infection especially mycetoma
- Trauma to the lungs / lung contusion
- Pulmonary artero-venous malformation
Causes of diffuse pulmonary haemorrhage:
This usually involve the small vessels in the lungs- Autoimmune diseases and vasculitis (Wegener Granulomatosis, Goodpasture syndrome, sistemic lupus erythematosis, Henokh-Schonlein Purpura)
- Pulmonary Hypertension
- Heart diseases with pulmonary edema
- Antikoagulant and thrombolytic agent
- Pulmonary haemosiderosis
Symptoms
Symptoms depends on the underlying diagnosis. Patient may presented with:
- Difficulty breathing
- Chest pain
- Fainting
- Rapid heart rate
- Cough up blood
- Unable to lie flat
- Wake up in the middle of the night due to coughing
- Swelling of the legs and ankles
Complications
- Right heart failure
- Irregular heart rhythm ( arrythmias)
- Blood clot
- Bleeding into the lungs
- Death
Treatment
Treatment is according to the underlying diagnosis
- Pulmonary embolism
Blood clots to the lungs are treated with blood thinners (anticoagulation). The most often used medicines are heparin, low molecular weight heparin or factor X inhibitor in acute setting and long term warfarin for about 6 months or more. - Pulmonary hypertension
The aim of treatment is to improve quality of life. Conventional treatment options include:- Oxygen Therapy In Cases Of Hypoxaemia,
- Anticoagulants Such As Warfarin,
- Digoxin
- Diuretics In Cases Of Rightsided Heart Failure.
Several medicines can lower blood pressure in the pulmonary arteries. However, these drugs have been best shown to improve idiopathic pulmonary arterial hypertension. Eg:
- Bosentan
- Sildenafil
- Epoprostenol
- Pulmonary edema
- Fluid restriction
- Diuretics: furosemide and spironolactone
- Angiotensin-converting enzyme (ACE) inhibitors: perindopril, enalapril, ramipril
- Beta-blockers: metoprolol and carvedilol
- Vasodilators that reduce blood pressure: amlodipine, hydralazine and isosorbide mononitrate
- Pulmonary hemorrhage
Treatment of pulmonary is depending on the quantity of the blood coughed up and the cause of bleeding. For example, pneumonia and lung abscess require antibiotics, while tuberculosis require anti tuberculosis drugs. Autoimmune diseases and vasculitis requires immunosuppressive drugs. ( refer haemoptysis)
Prevention
General prevention is Lifestyle changes such as:
- Quit smoking
- Follow a healthy diet
- Exercise
Specific prevention related to the underlying diagnosis:
Pulmonary embolisms can be prevented through drugs that break up blood clots before they reach the lung, physical activity, compression socks that improve blood circulation in the legs, pneumatic compression (a massage or compression of the legs through use of an electronic cuff) and thrombolytic agent.
| Last Reviewed | : | 21 May 2015 |
| Writer/Translator | : | Dr. Zamzurina bt. Abu Bakar |
| Accreditor | : | Dr. Azza bt. Omar |