What is Respiratory Distress Syndrome (RDS)?
Respiratory distress syndrome (RDS) in the newborn, also known as hyaline membrane disease, is a common complication seen in premature babies. Babies with this condition will develop breathing difficulty and may require intensive care management. RDS can be mild or severe, the severity and progression depend mainly on lung maturity.
Whom does it affect? Risk factors for neonatal RDS:
The earlier a baby is born the chances for the baby to develop RDS is higher as surfactant is likely to be deficient and immature in the lungs. Researches have shown that on average, a developing baby’s lungs are considered to be mature and fully functional around 35 to 36 weeks of gestation. For babies born before that, breathing can be a serious challenge.
There are other risk factors besides prematurity as the main cause for RDS. They include babies of diabetic mothers, history of previous siblings with RDS, multiple births (like twins), complicated deliveries, and caesarean deliveries without labour and male gender.
What causes RDS?
In healthy babies the lungs small air-exchange sacs (called alveoli) are coated by surfactant. Surfactant is a soap-like greasy material which makes the lung surfaces slippery. When the baby takes the initial first breath the air sacs expand, and filled with air and because of the slippery property of the lung surface; the air sacs remain open even when baby breathes out (exhales) and easily reinflate when baby breathes in.
Surfactant usually appears in the lungs at about 24th weeks of pregnancy. It gradually builds up fully by the 37th weeks. RDS is due to deficiency and immaturity of surfactant along with structural immaturity of the lungs, making breathing very difficult and inefficient. The earlier a baby is born, the less-developed the lungs are and the higher the chance of RDS.
How does RDS progress?
RDS usually begins shortly after birth and increases in severity over the first 2 days. A baby with RDS is likely to develop difficulty or rapid breathing in order to eliminate carbon dioxide (waste breathing product) , noisy breathing (grunt), chest wall retractions and may appear blue (cyanosis) due to inadequate oxygenation.
The baby may require more support for the initial 2 to 3 days. Baby will start to improve with the adequate support and as the lung starts to produce more surfactant.
How is RDS diagnosed?
RDS is frequently diagnosed in premature babies, as lung immaturity is the most common cause of RDS. A baby with RDS may develop the following signs:
- Rapid breathing to eliminate the waste product of breathing.
- Grunting, a noise produced when the baby tries to exhale through a closed glottis to open up the collapsed alveoli.
- Chest wall indrawing / collapsing inward with each breath.
- Bluish tinge of the skin (cyanosis), which indicates oxygen insufficiency in the blood.
Presences of all the above signs are not specific for RDS as they are also seen in other causes of breathing problems like lung infection.
Tests / Investigations carried out
-
Chest X-ray may need to be carried out in order to confirm the diagnosis of RDS. It is likely to show small lung volume and “ground glass” appearance (Figure 2).

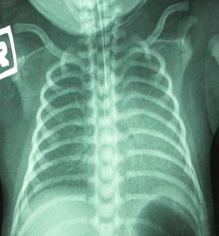
Figure 1: Chest X-ray of normal lung Figure 2: Respiratory distress syndrome - Blood gases are useful to measure the level of oxygen, carbon dioxide and acid in the blood which may indicate severity of the RDS
- Pulse oximetry is a non-invasive oxygen monitor commonly used in the intensive care, which is seen as a small light attached to the baby’s hand or foot to measure the body oxygen level. The baby’s blood will also be tested for the possibility of infections like blood stream infection or lung infection (pneumonia) which may accompany RDS.
How do we prevent RDS?
The most effective way to prevent RDS is by preventing premature birth which is by far the most common cause of RDS. Early and good antenatal care plays an important role as this will result in healthy mums, healthier babies and fewer premature births.
Judicious decision of caesarean-sections, avoiding unnecessary or poorly-timed caesarean-sections will also play an important role in reducing RDS risk.
If the birth cannot be delayed beyond 34 weeks, the mother may be given corticosteroid therapy before birth. Corticosteroids (like Dexamethasone) may help in developing lung maturity. Corticosteroid is often given to pregnant mum with risk of early delivery between 24 and 34 weeks of pregnancy. For effective treatment, 2 doses of corticosteroid should be administered, with the first dose given at least 24 hours prior to delivery. This therapy will reduce the rate and severity of RDS as well as the rate of other complications of prematurity.
How do we treat newborn with RDS?
High-risk cases like the premature baby with RDS will develop breathing difficulty shortly after birth; therefore prompt medical attention by the neonatal resuscitation team will be needed.
Babies with mild RDS can be treated with NCPAP (nasal continuous positive airway pressure – Figure 3). Babies with more severe disease are treated with mechanical ventilation (Figure 4) and surfactant replacement therapy.
|
|
|
| Figure 3: NCPAP | Figure 4: Intubation & Ventilation |
It is important that all babies with RDS receive good supportive care, including gentle handling, well maintained body temperature, careful fluid management, adequate nutrition and prevention of infection.
References:
- Nelson Textbook of paediatric 18th edition , Robert M. Kliegman, MD, Bonita M.D. Stanton, MD, Joseph St. Geme, Nina Schor and Richard E. Behrman.
- European Consensus Guidelines on the management of neonatal respiratory distress syndrome – 2010 updates , Neonatology 2010;97 : 402-417.
- Elective cesarean Section ; It’s impact on neonatal respiratory outcome, Clinical perinatology, 2008 June : 35(2) : 373 –iv , Ashwin Ramachamdrappa Dept of paeds university school of medicine Atlanta.
- Neonatal Outcomes of late – Preterm Birth associated or not with intrauterine growth restriction, Obstetric and Gynecology International, Volume 2010. Article ID 231842, Cristiane Ortigosa Rocha, Roberto Eduardo Bittar, and Marcelo Zugaib Dept of Obstetrics, University of Sao Paulo, Brazil.
- Neonatal respiratory distress syndrome , Medline : Daniel Rauch, MD, FAAP, Director, Pediatric Hospitalist Program, Associate Professor of Pediatrics, NYU School of Medicine, New York, NY.
- Antenatal steroids in preterm labour for the prevention of neonatal deaths due to complications of preterm, International Journal of epidemiology 2010:39 – 122 i33, Judith Mwansa- Kambafwile et al, Dept Public Health, Faculty Of Health sciences, University Cape Town, south Africa.
- Neonatal respiratory distress: recent progress in understanding pathogenesis and treatment outcomes, Korean journal of pediatrics Vol.53, no1, and 20: So young Kim, Dept of pediatrics, College of Medicine. The Catholic University of Korea;Seoul, Korea.
- Respiratory Distress Syndrome , About kids health, Children Hospital for the sick, Andrew James MBChB, MBI, FRACP,FRCPC & Jaques Belik, MD, FRCPC.
- Textbook of Perinatology ;10-15, E Saling.
- Quality Improvement in respiratory care: Decreasing BPD Robert H. P fister et al Dept of Pediatrics, The University of Vermont, Burlington, VT, USA Clin Perinatol 37 (2010) 273–293.
| Last reviewed | : | 28 August 2020 |
| Writer | : | Dr. Ang Ee Lee |
| Reviewer | : | Dr. Zainab bt. Kusiar |









