Introduction
Radiotherapy uses radiation such as x-rays, gamma rays, electron beams or protons to kill or damage cancer cells and stop them from growing and multiplying. It is a localized treatment, which means it generally only affects the part of the body where the radiation is directed. The radiotherapy treatment planning is used to obtain optimal balance between delivering a high dose to target volume and a low dose to intervening tissues. International guidelines such as Quantitative Analysis of Normal Tissue Effects in the Clinic (QUANTEC) allowing the clinician to limit the dose to normal tissue as much as possible and reasonably categorize toxicity raised based on dose/volume parameters. Although the radiation can also damage normal cells, they can usually repair themselves.
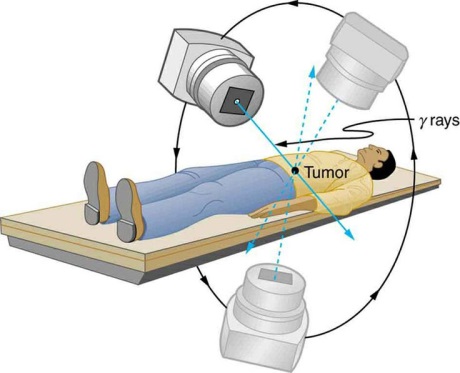
Figure 1 : Radiotherapy uses radiation to kill and damage targeted cancer cells while sparing surrounding normal tissues. (Image source: www.pinterest.com)
The Accident
The radiation accident that led to the death of Mr. Scott Jerome-Parks in New York has been much in the news. In March 2005, the hospital failed to detect a computer error that directed a linear accelerator to blast Mr. Jerome-Park’s brainstem and neck with beams of radiation on three consecutive days. The fatal overdose left him burned, deaf, struggling to see and unable to swallow. This accident has become an eye opener in medical field related to radiation.
Safety and Precautions
It is well known that radiation saves countless lives, and serious accidents are rarely happened. While new technology grows, its complexity has created new avenues for error. That is why a very high level of accuracy is needed during radiotherapy treatment. Within acceptable ranges of good practice and equipment performance, the prescribed dose should be delivered to the tumour while minimizing the doses to other tissues and organs.
All therapeutic exposures to ionizing radiation are subject to the principles of justification and optimisation. The decision to perform a radiotherapy procedure rests upon a professional judgement of the benefit to the health of patient, while accounting for any biological effects that might be caused by the ionizing radiation.
The Team
A successful and safe treatment requires a treatment team including oncologists, medical physicists, radiation therapists and nurses.
The oncologists will advise about treatment options and consent for treatment if patients are agreed. They will determine what area to treat, total dose, fractionation and added measures such as dental review and concurrent chemotherapy. Together with physicist/dosimetrist, oncologist determines what techniques to use to deliver the prescribed dose. The physicist/dosimetrist then makes detailed treatment calculations to achieve prescription.
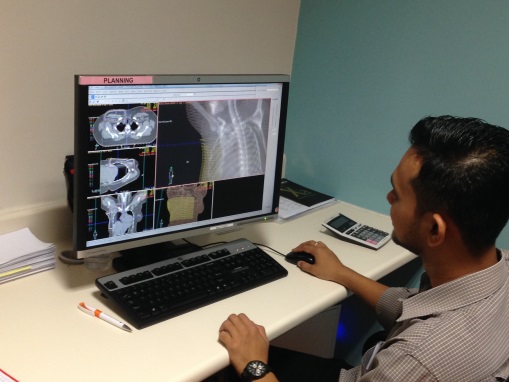
Figure 2 : Treatment calculations and dose optimization for radiotherapy are run by computer system called treatment planning system (TPS).
Radiation therapists are specially trained technologists who acquire images and deliver the daily treatment. During CT-simulation, therapist will setting up the patient in a reproducible position using appropriate immobilisations to minimise movement and for patient’s comfort. The same set up position will be used for daily treatment. The conventional method to attain positioning reproducibility is to use skin marks together with room lasers. Patients are often immobilised with thermoplastic masks.

Figure 3: Radiotherapy Head and Neck Mask. The mask helps to keep the head and neck from moving so that the patient will be in the exact same position for each treatment.
Frequent imaging is done during a course of radiation therapy for the purpose of improving the precision and accuracy of the treatment. Using specialized computer software, these images are then compared to the reference images taken during CT-simulation. Any necessary adjustments are then made to the patient’s position in order to achieve more precisely target radiation.
Physicist will make sure the radiation equipment is working at its best to deliver the right doses to the patients by doing scheduled Quality Control (QC). QC is the regulatory process through which the actual quality performance is measured, compared with existing standards and finally the actions necessary to keep or regain conformance with the standards. The licensee shall follow the Quality Assurance Programme (QAP) in Radiotherapy under the Atomic Energy Licensing Act 1984 (Act 304), Ministry of Health, Malaysia dated on July 2012. Other standards that being followed are AAPM Task Group Report: TG 142 for linear accelerator (LINAC) and AAPM Task Group Report: TG 148 for Tomotherapy machine.
Patient-specific QA was done to verify that the treatment parameters which are sent to the treatment unit are consistent with the approved plan. Dose verifications are done by comparing calculations and measurements of the dose in a phantom irradiated in accordance with a specific treatment plan.
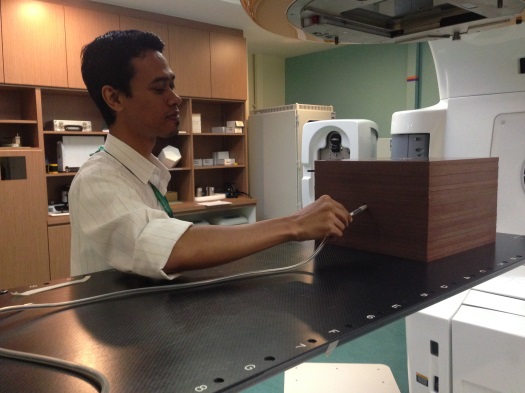
Figure 4 : Patient-specific QA is done by a physicist using solid water phantom for point dose measurement.
Patient’s Care
For patient side, there are some practical things to consider. Before you give your consent for radiotherapy, you need to confirm that you are not pregnant and understand you should avoid becoming pregnant during treatment. This is because the radiation from the treatment could harm a developing foetus. For male patient, you are advice not to father a child during treatment and for a few months after the treatment finished.
If you have a pacemaker, implantable cardiac devices or cochlear implant, please tell your oncologist. These devices can be affected by radiotherapy, so the treatment has to be planned to allow them. Stopping smoking during and after radiotherapy is very worthwhile. Research has shown that, smoking may make the treatment less effective, as well as increasing the side effects.
As radiotherapy affects people in different ways, it’s difficult to predict exactly how someone will react to the treatment. Most side effects disappear gradually once the course of the treatment is over; but for some people, they may continue for a few weeks. Being aware of side effects in advance can help patient to cope with any that may occur.
References
- Jatinder R. Palta, Ph.D. (2015). Modern-Day Linear Accelerator Acceptance Testing and Commissioning.
- Walt Bogdanich. (2010,January 23). Radiation Offers New Cures, and Ways to Do Harm. Retrieved from http://www.nytimes.com
- Macmillan Cancer Support. (2015). Understanding Radiotherapy : Before Your Radiotherapy. http://www.macmillan.org.uk
- Martin D. Abeloff, James O. Armitage, Allen S.Lichter, John E. Niederhuber, eds New York (NY). (2000). Clinical Oncology, Second Edition. Churchill Livingstone.
- Medscape: A Long Time Coming: New Guidance on “Normal Tissue Effects” for Radiation Oncology. (15 April 2010).
| Last Reviewed | : | 15 March 2017 |
| Writer | : | Fatin Humaizah bt. Abd Moin |
| Accreditor | : | Yusnira bt. Yusoff |







