Introduction
Orthodontic treatment correct irregular arrangement of teeth by using fixed or removable appliances (braces). Apart from its aesthetic effect, this treatment has the potential to cause unwanted side-effects. The side-effects can be:
- Intra oral (inside the mouth)
- Extra oral ( outside the mouth)
- Systemic (the whole body)
Intra oral effects
Side-effects in the mouth include:
- Effects on the teeth
- Effects on the periodontium (gum tissues)
- Effects on the soft tissues
Effects on the teeth
-
Decalcification effects on the enamel surfaces of the teeth can be seen as white spot lesions. This is the most common complication (Figure 1). Decalcification of the enamel surface is due to acid produced from bacterial plaque metabolism.(Kidd & Smith;1991)

Figure 1: Decalcification of the tooth surfacesThe decalcification process can occur very fast, often within a month of orthodontic treatment with fixed appliances. Therefore, it is very important for patients to maintain excellent oral hygiene. Patients are advised to reduce their intake of acidic or fizzy drinks such as carbonated drinks which are known for their decalcification effects.
Gorelick et al. (1982) found that, 50% of patients wearing braces had white spot lesions on their tooth surfaces after orthodontic treatment. The most common teeth affected are upper lateral incisors (23%). However, the duration of orthodontic treatment does not affect the incidence or number of white spot lesions.
-
Tooth caries or decay easily occur if oral hygiene is very poor and/or the length of treatment is too long.
-
Attrition (worn off) of the enamel surfaces of the teeth may occur due to the fixed ceramic or metal brackets; for instance, when the tip of the upper canine tooth is in contact with the bracket on the lower teeth during tooth movement (Figure 2). Ceramic brackets placed on the lower incisor (front) teeth may also cause attrition to the upper incisor teeth (Swartz; 1988).
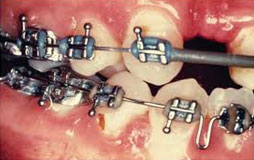
Figure 2: Attrition of to the upper canine tooth -
Root resorption (shortening) can occur during orthodontic treatment (Figure 3). Root resorption usually take place on the apical and lateral root surfaces especially on upper and lower incisor teeth.
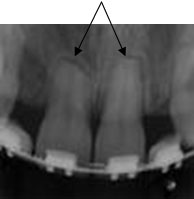
Figure 3: Periapical radiograph shows root resorption of upper central incisor teethThe mechanism of root resorption is still not very clear. Excessive orthodontic forces may cause hyalinization of the periodontal ligament and increase bone cell activity especially cementoclasts and osteoclasts causing root resorption. (Breznik & Wasserstein;2002)
Other risk factors of root resorption include :
- Pipette-shaped root – root resorption may easily occur ( Malmgren;1998)
- Teeth with history of trauma and/or had root canal treatment are more prone to root resorption (Drydale et al;1996)
- Treatment of the impacted canine tooth may increase the risk of root resorption to the lateral incisor and first premolar teeth. This is due to the long treatment time and long pathway of eruption of the canine.(Woloshyn et al;1994)
- Mechanics of orthodontic treatment – treatment with ‘rectangular’ archwires (Linge & Linge;1983), Class II elastic traction (Levander & Malmgren; 1988), intrusive tooth movements, long ling pathway of tooth eruption and excessive stress/traction forces on teeth increase the tendency for root resorption (Kaley & Philips; 1991).
- Habits like bruxism (grinding of teeth) and nail biting may stress the teeth causing root resorption
- Age – patients more than 11years old are at higher risk for root resorption (Linge & Linge; 1983). Adult patients with short roots are also more prone to root resorption.
- General factors which may increase risk of root resorption :-
- Female > male
- Long treatment time
- Systemic factors eg. Para /hyperthyroidism
-
Pulpitis or inflammation of the tooth pulp was found in 90% of orthodontic patients, especially during the first month of treatment (Anstendig & Kronman; 1972). Although the patient may experience pain, pulp inflammation will not devitalize the tooth.
Effects on the periodontium (gum tissues)
Oral hygiene maintenance may become more complicated with orthodontic appliances (braces) and bacterial plaque accumulation can easily occur on the gum tissues.
- Plaque accumulation will cause gum inflammation (gingivitis). Almost all orthodontic patients will experience gingivitis. (Boyd & Baurmind; 1992)
- Gum recession (thinning) may occur if tooth movement is uncontrolled during orthodontic treatment
- Gingival hyperplasia (gum swelling) can occur due to poor oral hygiene (Figure 4)
- Resorption/reduction of alveolar crestal bone may occur but is usually minimal. It may become worse if the patient has a history of bone resorption prior to orthodontic treatment.

Figure 4: Gingival Hyperplasia
Patients who have gum disease before orthodontic treatment should pay more attention to oral hygiene maintenance to prevent further complications to their gum tissues
Effects on the soft tissues
Mucosal soft tissues of the mouth include the upper and lower lips, inner part of the cheek, palate, floor of the mouth and tongue.
Traumatic effects on the soft tissue mucosa may occur as ulcers. This may be due to over-extended ends of the archwire, brackets on the labial surface of the teeth (Figure 5) and orthodontic bands on the molar teeth. (McGuinness; 1992)

Figure 5: ulcer due to orthodontic brackets
Soft tissue allergy due to orthodontic components containing nickel and iron is not common. About 5-12 times more of nickel concentration is needed to have an allergic effect on the oral soft tissue than on the skin (Dunlop et al; 1989). Nevertheless, closer attention should be given to those who have had previous allergy to nickel.
Soft tissue allergy may also occur due to ‘latex’ (rubber) in the elastomeric components or gloves used by the operator.
Extra-oral effects
Side-effects of orthodontic treatment outside the mouth is uncommon. Some of the possible effects may include:

Figure 6: Allergic reaction around the mouth
- Allergy to orthodontic appliances containing nickel is the most common. Patients may also be allergic to ‘latex’ gloves worn by the operator or to materials used in the treatment (Hutchinson: 1994)
- Headgear use during orthodontic treatment may cause injury to the face, eyes and mouth due to the sharp ends of the headgear (Holland et al; 1985).
- Injury to the temporomandibular joint – temporomandibular dysfunction (TMD) (Sadowsky; 1992)
Systemic effects
Very rare.
-
Cross infection may occur if the instruments used during orthodontic treatment are not completely sterile.
Infective Endocarditis may occur if the patient has heart valve disease (Robert et al; 2000)
Conclusion
Although iatrogenic side-effects of orthodontic treatment can occur, it is uncommon to cause serious injury to the patient. Therefore, it can be concluded that patients with severe malocclusions will still benefit from the treatment compared to those with mild malocclusions.
References:
- Anstendig H & Kronman J; 1972 A histological study of pulpal reaction to orthodontic tooth movement in dogs, AO, 42;50-55
- Boyd RL & Baurmind S; 1992 Periodontal considerations in the use of bonds or bands on molars in adolescents and adults, AO, 62;117-126
- Brezniak N & Wasserstein A; 2002a,b Orthodontically induced inflammatory root resorption: Part I & II: The clinical aspects, AO, 72;175-184
- Drysdale D et al; 1996 Orthodontic management of root-filled teeth, BJO, 23;255-260
- Dunlap CL et al; 1989 Allergic reaction to orthodontic wire: Report of a case, JADA, 118;449-456
- Gorelic L et al; 1982 Incidence of white spot formation after bonding and banding, AJO, 81;93-98
- Holland G et al; 1985 Severe ocular injuries from orthodontic headgear, JCO, 19;819-825
- Hutchinson I; 1994 Hypersensitivity to an orthodontic bonding agent. A case report, BJO, 21;331-333
- Kaley JD &Phillips C; 1991 Factors related to root resorption in edgewise practice, AO, 61;125-131
- Kennedy DB et al; 1983 The effect of extractions and orthodontic treatment on dentoalveolar support, AJO, 84;183-190
- Kid E A M & Smith B G N; 1991 Pickard’s Manual of Operative Dentistry, 6th edition , Oxford Medical Publications, Oxford
- Levander E & Malmgren O; 1988 Evaluation of the risk of root resorption during orthodontic treatment: A study of upper incisors, EJO, 10;30-38
- Linge BO & Linge L; 1983 Apical root resorption in upper anterior teeth, EJO, 5;173-183
- Malmgren O et al; 1982 Root resorption after orthodontic treatment of traumatized teeth, AJO, 82;487-491
- McGuinness N; 1992 Prevention in orthodontics- A review, Dent Update, 19;168-175
- Roberts RG et al; 2000 Bacterial endocarditis & orthodontics, J R Coll Surg Edin, 45;141-145
- Sadowsky C; 1992 The risk of orthodontic treatment for producing temporomandibular disorder: A literature review, AJODO, 101;79-83
- Swartz ML; 1988 Ceramic brackets, JCO, 22;82-88
- Woloshyn H et al; 1994 Pulpal and periodontal reactions to orthodontic alignment of palatally impacted canine, AO, 64;257-264
| Last Reviewed | : | 28 Ogos 2020 |
| Writer | : | Dr. Sharina bt. Sharudin |
| Translator | : | Dr. Yatimah bt. Othman |
| Accreditor | : | Dr. Loke Shuet Toh |
| Reviewer | : | Dr. Hjh. Rashidah bt. Dato’ Hj. Burhanuddin |







