Introduction
Assisted reproductive technology (ART) are methods used to achieve pregnancy. It is reproductive technology used primarily for infertility treatments (also known as fertility treatment).Examples of ART include in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), cryopreservation and intrauterine insemination (IUI).IVF and ICSI are currently used to treat many fertility problems including unexplained infertility, male infertility and failure of conventional treatment. There are two main laboratories running out ART procedures, which is Andrology and Embryology laboratory.
A typical IVF/ICSI cycle consists of a seven-phase process:
1) Ovarian Stimulation and Monitoring
2) Egg Retrieval
3) Semen Collection and Processing
4) Insemination and Fertilisation
5) Embryo Development and Embryo Selection
6) Embryo Transfer
7) Luteal Phase and Pregnancy
Ovarian Stimulation and Monitoring
There are two main protocols for controlled ovarian stimulation. The most common one is a long GnRH (Gonadotropin-releasing hormone) agonist protocol where the secretion of pituitary FSH and LH hormones is suppressed in order to prevent premature ovulation. Once optimal suppression is achieved, daily injections of gonadotropin are needed to recruit multiple follicles. The injections continue for about 12-14 days, and the dose and combination of medications are depends individually ovarian response. Ultrasound imaging and hormone assessments are used to monitor follicular development. When the lead follicles have reached the appropriate size, the final maturation of eggs is done by hCGadministration. Egg retrieval is scheduled 34-36 hours after hCG injection.
While in a short GnRH antagonist protocol it must be adapted to the spontaneous onset of the menstruation but has shorter cycle lengths and less risk of ovarian hyperstimulation syndrome(OHSS).GnRH antagonist protocol has overall better results for expected poor and hyper-responders.
Egg Retrieval
Egg retrieval is performed under intravenous sedation or general anaesthesia and usually takes between 20 to 40 minutes, depending on the number of mature follicles. Ovarian follicles are aspirated using a needle guided by trans-vaginal ultrasonography. Follicular fluids aspirated are then scanned by the embryologist to locate all available eggs. The eggs will be placed in a special media and cultured in an incubator until insemination.
Semen Collection and Processing
Semen sample is collected on the day of egg retrieval procedure. Prior the day to give sample, abstinence about 2-5 days is required. Sample is usually produced through masturbation. Once semen sample is liquefied, analysis and sperm processing will be done. The most common method used to process sperm sample is called density gradient preparation. The semen is added to a test-tube that contains a special media, which filters out sperm that have poor motility. If the sperm count isn’t ideal, or if the man has had a surgical sperm collection, the sperm sample will be spun toconcentrate as many sperm together as possible. Those processed samples are then leaving in incubator until insemination.
Insemination and Fertilisation
There are two different types of insemination techniques which are IVF standard insemination or ICSI (Intracytoplasmic Sperm Injection). IVF standard insemination is used in patients that have normal sperm parameters. Approximately 50,000 to 100,000 motile sperm are transferred to the dish containing the eggsand leaving them overnight so that fertilisation can occur. If there are severe problems with the sperm, or if IVF standard insemination has failed previously, ICSIis an option.
ICSI procedure is a specialized form of fertilisation which is performed under a high-powered microscope. The embryologist picks up a single spermatozoa using a fine glass micro needle and injects it directly into the egg cytoplasm. ICSI increases the chance that fertilisation will occur if the semen sample has a low sperm count and/or motility, poor morphology or poor progression. If there are no sperm in the ejaculate, sperm may be obtained via a surgical procedure. ICSI is always used to achieve fertilisation if the sperm is surgically retrieved.
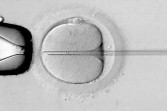
Intracytoplasmic Sperm Injection (ICSI) is a procedure where a single spermatozoa is being injected into a mature egg’s cytoplasm.
The sign of fertilisationcan be assessed 18 to 20 hours post insemination for IVF and 16 to 18 hours for ICSI. Normal fertilisation can be identified only when there have two pro-nuclei appear on the egg cytoplasm. The fertilised eggs are then continued culture in incubator until they are ready to be placed back into the uterus.

Abnormal fertilisation. Three pro-nuclei are found and seen in the center of egg’s cytoplasm.

A normally fertilised egg is called a zygote. Two pro-nuclei are seen in the center of egg’s cytoplasm.
Embryo Development and Embryo Selection
Embryos can be grown in the laboratory for up to six days after egg retrieval. There are two different stages of embryo culture and transfer, either ‘cleavage stage’ or ‘extended/ blastocyst stage’. ‘Cleavage stage’ is the term used for either day two or day three embryo and usually has approximately 4-8 cells. Besides, not only the number of cells is assessed, the cell symmetrical and fragmentation are also assessed. Fragmentation occurs when the cells divide unevenly resulting in cell-like structures which crowd the embryo. ‘Cleavage stage’embryo culture and transfer is beneficial for couples that have low numbers and/ or poor quality of embryos available for transfer.
‘Extended/ blastocyst’ stage is the term used for either day five or day six embryo. At this stage the embryos have increased in size and are even more developed. They resemble a ball of cells with fluid inside. The more expanded is the better the quality of the embryo. ‘Blastocyst stage’ embryo has a higher potential for implantation and fewer embryos are being chosen to transfer on day 5 and this reduce the chance of multiple pregnancies.
Embryo on ‘cleavage stage’ (day-2 and day-3):

a) 2-cells embryo

b) 4-cells embryo

c) 8-cells embryo
‘Extended/ Blastocyst stage’embryo (day 4, day 5 and day 6):

d)Morula
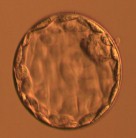
e)Expanded Blastocyst

f)Hatching Blastocyst
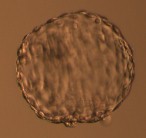
g)Hatched Blastocyst
Embryo Transfer
Embryos are transferred on day 3 when they are at the cleavage stage (6-8 cells) or on day 5 when they have reached the blastocyst stage. The exact number transferred will depend on a woman’s age and embryo quality. Generally one or two embryos will be transferred to the uterus. It is important to note that the risk of multiple pregnancy increases with the number of good quality embryos transferred. The remaining embryos will be frozen for future use.
Embryo transfer is a simple procedure that does not require any anaesthesia. Embryos are loaded in a soft catheter and are placed in the uterine cavity through the cervix. The catheter is then slowly removed and checked under the microscope to ensure that there are no embryos remaining.
Luteal Phase and Pregnancy
The Luteal Phase is the 2 weeks period between the embryo transfer and the pregnancy test.Luteal support is the administration of medication, generally progesterone, progestins or GnRH agonists, to increase the success rate of implantation and early embryogenesis, thereby complementing and/or supporting the function of the corpus luteum. Sexual intercourse should be avoided for about one week. After 16-days post transfer, a blood test ?-hCG shall be done to determine whether a pregnancy occurred.
Reference
-
Edwards RG, Brody SA: Principles and Practise of Assisted Human Reproduction. WB Saunders Company, 1995.
-
Nagy ZP, Varghese AC, Agarwal A: Practical manual of in vitro fertilization. Springer: USA, 2012.
-
Patrizio P, Tucker MJ, Guelman V: A color atlas for human assisted reproduction. Laboratory and clinical insights. Lippincott Williams & Wilkins: USA, 2003.
-
Prakash, T., Priti, P. T.: The heart and soul of ART ……is in the laboratory. Jaypee Brothers Medical Publishers: India, 168-205, 2004.
| Last Reviewed | : | 10 Mac 2015 |
| Writer | : | Helen Tang Hoay Loon |
| Translator | : | Helen Tang Hoay Loon |
| Accreditor | : | Krishnan a/l Kanniah |







