What is a temporomandibular joint (TMJ) disorder?
Temporomandibular joint disorder is a general term to describe several conditions of pain and dysfunction of the muscles of mastication (chewing muscles) and the temporomandibular joints (the joints which connect the jaw to the skull). It is usually a benign condition that is not harmful. It usually affects one side of the jaw joint and rarely affects both sides. Many people may have some symptoms of TMD and in a small number it causes pain that affect daily functions that require examination and some form of treatment by dentist/dental specialists.
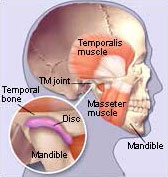
Image source : www.webmd.com
Figure 1: Schematic diagram of a Temporomandibular (TM) joint
What are the symptoms of TMD?
Generally, there are three cardinal symptoms of TMJ disorders which are facial pain, restricted jaw function and joint noise. The most common complain of patients with TMD is pain in the preauricular area (skin area in front of the ear). This pain may radiate to the neighbouring areas such the temporal (temples), frontal (forehead), or occipital area (back of head). The radiating nature may complicate the diagnosis as it may be felt as earache, headache or sometimes neck or shoulder pain. It is not surprising that many patient initially seek treatment from medical practitioners without any resolution of the symptoms.
Another common symptom that patient may also experience is limitation of mouth opening. It is usually caused by pain elicited or triggered in one or more of the masticatory muscles on the affected side upon wide mouth opening or during function. The limitation of mouth opening may also be associated with spasm (stiffness) of the masticatory (chewing) muscles that limit the jaw opening. In a small percentage of patients, ‘locked jaw’, a condition of inability to move the jaw during opening or closing may occur and signify a possibility of derangement of the internal part of the TMJ. In this condition, the joint disk which is a fibrocartilage membrane that cushions the articulating surfaces of the TMJ, is displaced from its position and interferes with joint movement. In a small percentage of reported chronic cases (prolonged symptoms), fibrosis (scarring) of the disk may occur that can cause more pain or jaw limitation.
Joint noises in TMD may presents as either clicking or crepitus. It is best heard by placing the index finger on the joint area during jaw opening or closing. The clicking sound if not associated with other TMD symptoms has no clinical significance and is commonly found in many of people.
In general, patients with TMD may experience one or more of these symptoms:
- Jaw pain or soreness that may be worse when you wake up or at night
- Jaw pain when biting, chewing or yawning.
- Clicking from your jaw joint when you move it.
- Stiffness or locking of your jaw joint.
- Earache or ringing in the ear (tinnitus).
- Difficulty opening and/or closing your mouth.
- Headaches.
What causes TMD?
The exact cause of TMD is not well understood. Generally, many studies show that TMD is closely associated with any activity that causes pain and inflammation of the joint and its muscles. Several triggering or aggravating factors includes bruxism, trauma, psychological stress; dental malocclusion, overuse or overextension of TM joint have been reported.
How is TMD diagnosed?
The majority of people actually do experience some form of TMD at one point or rather in their lives life. Most cases present with mild pain and are transient in nature, resolving over time with self-care therapy at home. In severe cases however, thorough examination by dentists/dental specialists is necessary to rule out more serious underlying problems. Several diagnostic procedures including radiographs, CT scans or MRIs may be required to detect presence of joint adhesion, degenerative joint diseases or other pathological changes. Sometimes assessment of patient’s psychological status is also needed.
How are TMJ disorders treated?
There is no single treatment modality that is actually effective for all patients with TMD. Treatment is mainly conservative, aiming to reduce the pain symptoms and to allow tissue healing to regain function. Rarely, surgery is needed and only reserved for severe cases that require corrective tissue repair by surgical procedures. Several conservative treatments commonly used are as the following:
Self-Care Practices at Home
There are steps that patients can take that may be helpful in easing symptoms, such as:
- Eating soft foods until symptoms lessen or diminished,
- Applying ice packs on painful area,
- Applying warm towel or heat pack on sore muscles,
- Avoiding extreme jaw movements (such as wide yawning, loud singing, and gum chewing),
- Learning and practicing techniques for relaxing and reducing stress,
- Practicing gentle jaw stretching and relaxing exercises that may help increase jaw movement.
- Usually a health care provider or a physical therapist may recommend exercises appropriate to patient’s need.
Medications
For many people with TMD, short-term use of mild pain medications is found to be very useful. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or diclofenac sodium, may provide adequate relief from jaw discomfort and act as an agent to reduce joint inflammation. If necessary, stronger pain medications may be prescribed. In some cases, muscle relaxants, or mild anti-depressants may be useful especially for chronic cases.
Stabilization Splints
Some dentists/dental specialists may recommend an oral appliance also called a splints or bite guards, which fits over the upper or lower teeth. However, there is inconclusive evidence with regards to its effectiveness. If a stabilization splint is recommended, it should be used only for a short time to avoid irreversible unwanted changes in the bite.

Figure 2: Splint for the lower arch
References
- Greenberg MS. Glick M (2003). Burket’s Oral Medicine Diagnosis & Treament (10th Ed). Hamilton.Ont: B.C Decker.
- Lis. T,Axelsson S Management of TMD: evidence from systematic reviews and meta-analysis. Journal of Oral Rehabilitation.May 2010:370(6): 430-51
- Neville BW, Damm DD,Alen CA, Bouquot JE (2002): Oral & Maxillofacial Pathology (2nd Ed.).Philadelphia: W.B.Sauders. pp. 75-79
| Last Reviewed | : | 19 June 2015 |
| Writer | : | Dr. Abdul Rahim bin Ahmad |
| Accreditor | : | Dr. Hans Prakash a/l Sathasivam |







