Introduction
What Is Trigeminal Neuralgia?
Trigeminal Neuralgia (TGN) is an extremely painful condition that affects the trigeminal nerve, one of the major nerves of the face and mouth. This nerve has three branches that provides sensory innervation for almost all of the face (Figure 1). TGN causes sudden episodes of extremely severe pain that lasts from a few seconds to a few minutes and can occur several times a day. The pain is usually described as stabbing or sharp shooting or electric shock like and is usually on one side of the face. It is a rare condition that is usually seen in patients above 50 years of age and is more frequent amongst women.
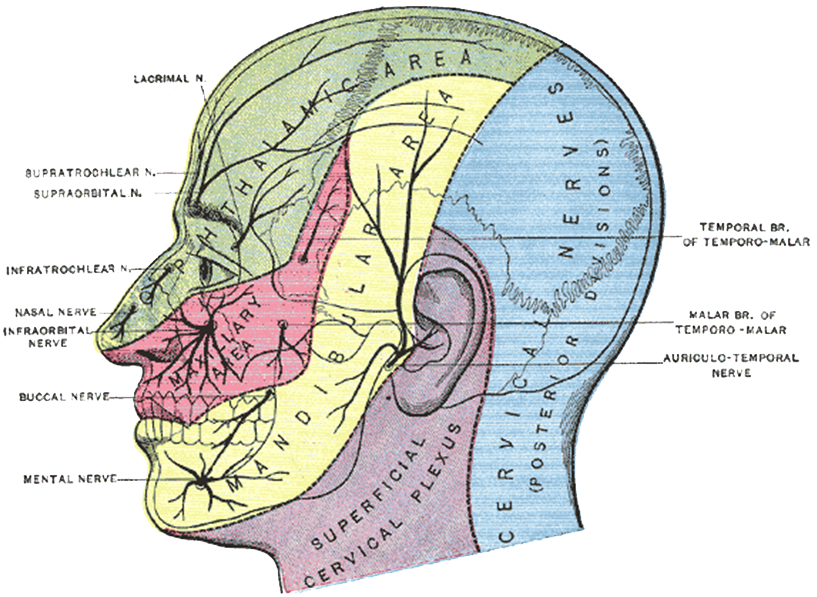
Figure 1: Distribution of the trigeminal nerve (green, red and yellow areas)
(Source : Reproduced from the 20th U.S. edition of Gray’s Anatomy of the Human Body)
What causes TGN?
The causative factor for TGN in most cases is unknown, however at times it can be due to compression of the nerve either by blood vessels or tumours (very rare). Some demyelinating diseases/conditions of the nerves can also cause symptoms of TGN.
What are the symptoms of TGN?
TGN manifests as sudden, sharp, shooting, lancinating, shock like pain over the face or mouth. These attacks usually lasts from few a seconds to a few minutes and can occur spontaneously or be triggered by certain activities.
The usual triggering activities for TGN would be:
- talking
- chewing, eating, drinking
- smiling
- light touch
- brushing teeth
- washing the face
- shaving
- face being exposed to the wind
TGN usually affects only one side of the face but very rarely it can affect both sides of the face. The pain experienced can be over the forehead, eye, cheek, lower jaw or upper jaw depending on which branch of the trigeminal nerve is affected. There may be accompanied facial spasm during the attacks. There is usually a pain-free period between attacks, however there are cases where even between attacks there is a dull aching pain. Patients also may find that touching particular areas over the face / mouth that can cause an attack to occur. These areas are known as “trigger zones”.
How is TGN diagnosed?
There is no absolute diagnostic test for TGN. As such, the diagnosis is largely dependent on the information given by the patient about the symptoms as well as the clinical examination performed by your attending physician. Some ancillary studies may be ordered by your doctor to help rule out other possible causes for the pain. The usual studies involved would be radiographs, MRI (magnetic resonance imaging) and some blood tests.
How is TGN treated?
Most cases of TGN are initially treated with medication to control / reduce the severity of the attacks. However, common pain medication such as paracetamol have not been found to very effective for the management of TGN. The most effective medication for management of TGN are anti-convulsants that are used to treat epilepsy. Unlike the usual pain medications (“pain-killers”), these medications usually need to be taken on a regular basis according to prescription and not only when there is pain.
The most commonly prescribed medication for TGN is carbamazepine. Although this medication is quite good at controlling the symptoms of TGN, there are patients who may not respond very well. As with most medications, carbamazepine does have the potential to cause some unwanted side-effects such as sleepiness and dizziness. In some patients it can cause severe skin reactions that will need emergency medical treatment. Some of the other medications that are commonly prescribed for TGN include gabapentin, phenytoin, baclofen, pregabalin and lamotrigine. At times, your doctor may prescribe a combination of medications to increase pain control and minimize unwanted side-effects.
Patients who have inadequate pain relief from medications or are unable to cope with the side-effects may be given the option of surgical intervention. The following are the different types of surgical intervention that may be performed:
- glycerol injection
- cryotherapy (freezing the nerve)
- peripheral neurectomy
- radiofrequency thermocoagulation
- microvascular decompression
- gamma-knife radiosurgery
These interventions will again depend on the patient, clinical as well as radiological findings. These procedures are usually done by a neurosurgeon who specializes in these procedures. Surgery may also be ineffective in some cases and the symptoms may return.
Can TGN Be Cured?
There is no known cure for TGN, however adequate pain control is usually achieved either with medication or surgery alone or in combination. TGN may also become asymptomatic for long periods of time.
Self – Care Measures
- If possible, avoid or reduce activities that trigger an attack. An example would be to using something to cover the face when going out in windy conditions.
- Maintain good oral hygiene and see the dentist regularly to avoid tooth related pain that may worsen the pain from the TGN.
- Inform your doctor of any adverse effects from your medication and if severe, seek immediate medical attention (this will be explained to you in much more detail by your attending doctor)
- Keeping a “pain diary” (to record the severity of pain, frequency of attacks, dosage and side-effects from medications) is useful for you as well as your doctor. This is useful when starting new medication or a new dosage of the current medication as it will record your progress as well as factors that may exacerbate or alleviate your condition.
- Tell your doctor is you feel unable to cope with your condition or if you feel sad. Patients with chronic pain can cause people to feel low, however there is treatment available.
References
- Classification Subcommittee of the International Headache Society: The international classification of headache disorders. Cephalalgia 2004, 24 (supplementary 1):1-160.
- Merskey H, Bogduk N: Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. Seattle: IASP Press 1994.
- Nurmikko TJ, Eldridge PR: Trigeminal neuralgia–pathophysiology, diagnosis and current treatment. Br J Anaesth 2001, 87:117–132.
- Love S, Coakham HB: Trigeminal neuralgia: pathology and pathogenesis. Brain 2001, 124:2347–2360.
- Sathasivam HP, Lau SH, Ahmad AR: A retrospective study of the Clinical Characteristics of Malaysian Trigeminal Neuralgia (TGN) Patients seen at the Oral Medicine Clinic, Kuala Lumpur General Hospital. Malaysian Dent Journal 2012
| Last Reviewed | : | 3 June 2014 |
| Writer | : | Dr. Hans Prakash a/l Sathasivam |
| Accreditor | : | Dr. Lau Shin Hin |







